COVID-19 (formerly known nCoV-2019)
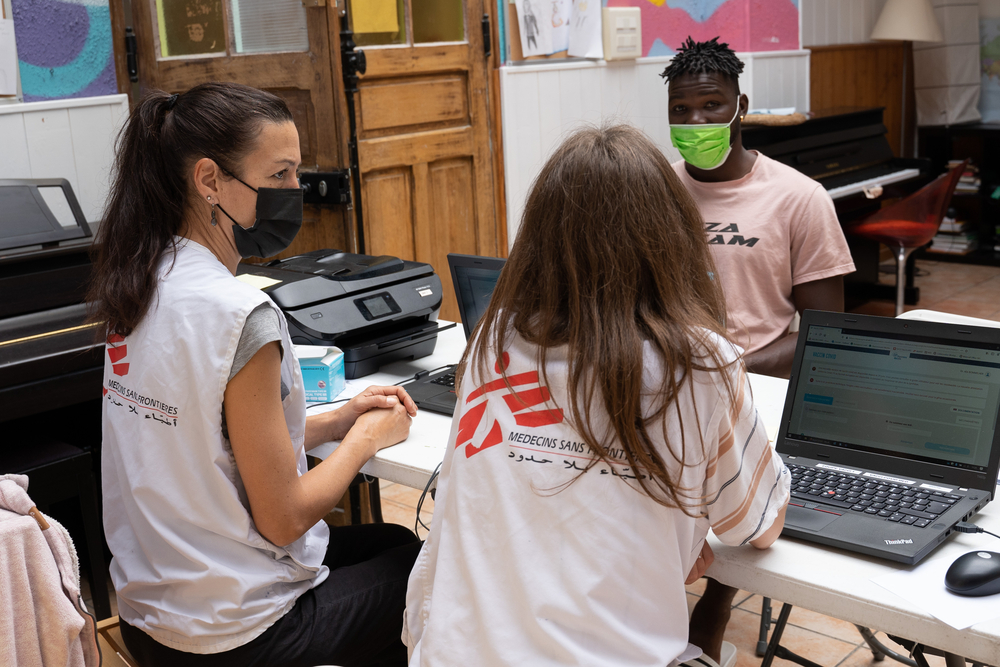
Doctors Without Borders/Médecins Sans Frontières (MSF) is following the fast-evolving development of the disease COVID-19 (formerly known nCoV-2019) it is a type of coronavirus. Specialized medical protective equipment from MSF is on its way to Wuhan Jinyintan Hospital in the capital city of Hubei province, China, the epicentre of the current coronavirus COVID-19 outbreak.
![]()
About the disease and virus:
What is the disease COVID-19?
The disease is called COVID-19 (short for Corona Virus Disease that emerged in 2019). It is caused by a virus which was discovered in early January in China and has been identified as a member of the family of coronaviruses. The virus seems to be transmitted through droplets spread by coughing that can be breathed in, or infect surfaces that people touch. This virus affects the respiratory system. The main symptoms include general weakness and fever; coughing and sometimes pneumonia and difficulty of breathing in a later stage. A runny nose and sneezing, that are often seen in other respiratory diseases like the flu or a cold, are rarer in COVID-19 patients.
What is known about the virus?
The virus was identified early January by Chinese scientists and is now called SARS-CoV-2, because of its similarities to the virus that causes SARS. The name of the disease caused by this new virus is COVID-19. The coronaviruses are a large family of viruses, most of which are harmless for humans. Four types are known to cause colds, two other types can cause severe lung infections (SARS and MERS) similar to COVID-19.
Like all viruses, SARS-CoV-2 needs cells of living beings to multiply itself. This virus seems to target cells in the lungs, and possibly other cells in the respiratory system too. Cells infected by the virus will produce more virus particles, which can then spread to other people by coughing, for instance.
How dangerous is the disease COVID-19?
Our collective understanding of the virus and the disease is still evolving. The latest estimates are that 80% of the people who get infected will only suffer from a mild or moderate form of disease. 15% will develop a severe form of the disease, which requires hospitalization. Some five percent will be critically ill. Sophisticated health care systems may be able to cure even the most critically ill patients, but the danger is that healthcare systems get overwhelmed by the large number of patients to be hospitalized, so those patients can’t access that level of care.
It’s clear that there are also infected people who show no or almost no symptoms of the disease. There are no good estimates of what percentage of infections these asymptomatic or pauci-symptomatic people make up of the total number of infections.
The disease is more dangerous for elderly people or people suffering from other infections or ailments, as often is the case with infectious diseases. More than 80% of the people who died of COVID-19 were over 60 years old, and over 75% had underlying medical conditions. Children, on the other hand, seem to be less affected by the disease, though they can still contract it. The mortality rates vary a lot from place to place, so it’s difficult to make a general point about how deadly COVID-19 is.
How contagious is the disease?
Our understanding of the virus and the disease is still evolving. The virus can be spread by coughing sick people. But it seems it can also be spread by people who have no or almost no symptoms. This doesn’t make the disease more contagious, but it makes it much harder to get a good picture of the way it’s spreading. It is unknown what percentage of all infections these ‘asymptomatic’ infections make up.
Many countries report exponentially growing figures of new cases, so the virus clearly has the potential to spread quickly. But many details about the infectivity of the virus are still unknown (how long it can survive in different circumstances outside the human body, how many viral particles are required for an infection, etc.).
For latest figures please see here: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
How can I prevent myself from being infected?
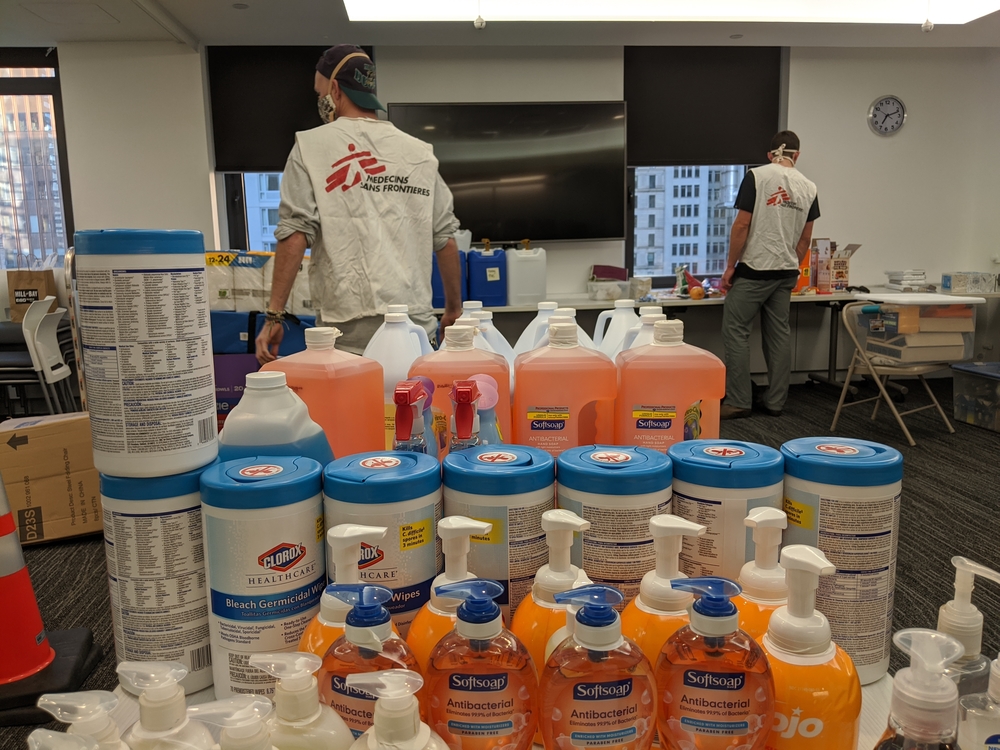
It’s important to protect yourself and protect others too. As with other coronaviruses, droplet infection seems to be the main mode of transmission. The virus enters the human body through the mouth or nose. This can happen by breathing in infected droplets, or by touching with your hands a surface in which droplets have landed, and then touching your mouth or nose later. Hence, simple infection control measures such as handwashing and cough and sneeze etiquette are effective and important for prevention.
Hand hygiene is paramount, so wash your hands often with soap and water. Use enough soap, and make sure all parts of both your hands are washed. Spend at least 20 seconds washing your hands. If there’s no visible dirt on your hands, an alcohol-based gel is also a good option.
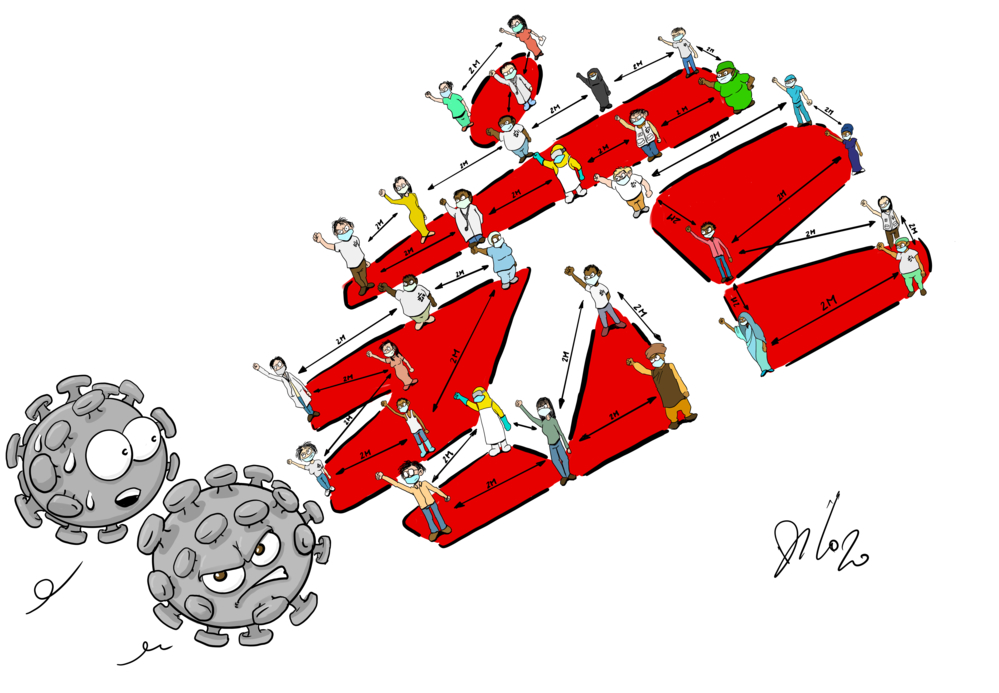
In places with local transmission of the virus, social distancing is advised. As the virus is passed on from person to person, not being too close to other person can prevent infections. Avoid crowded places and large gatherings.
If you cough or sneeze, cover your mouth and nose with a tissue, or with the inside of your elbow. Put used tissues in the bin immediately and wash your hands.
Given the current problems with the supply of masks and other protective equipment, healthcare staff should be prioritized.
Supporting prepardness efforts to fend off COVID-19
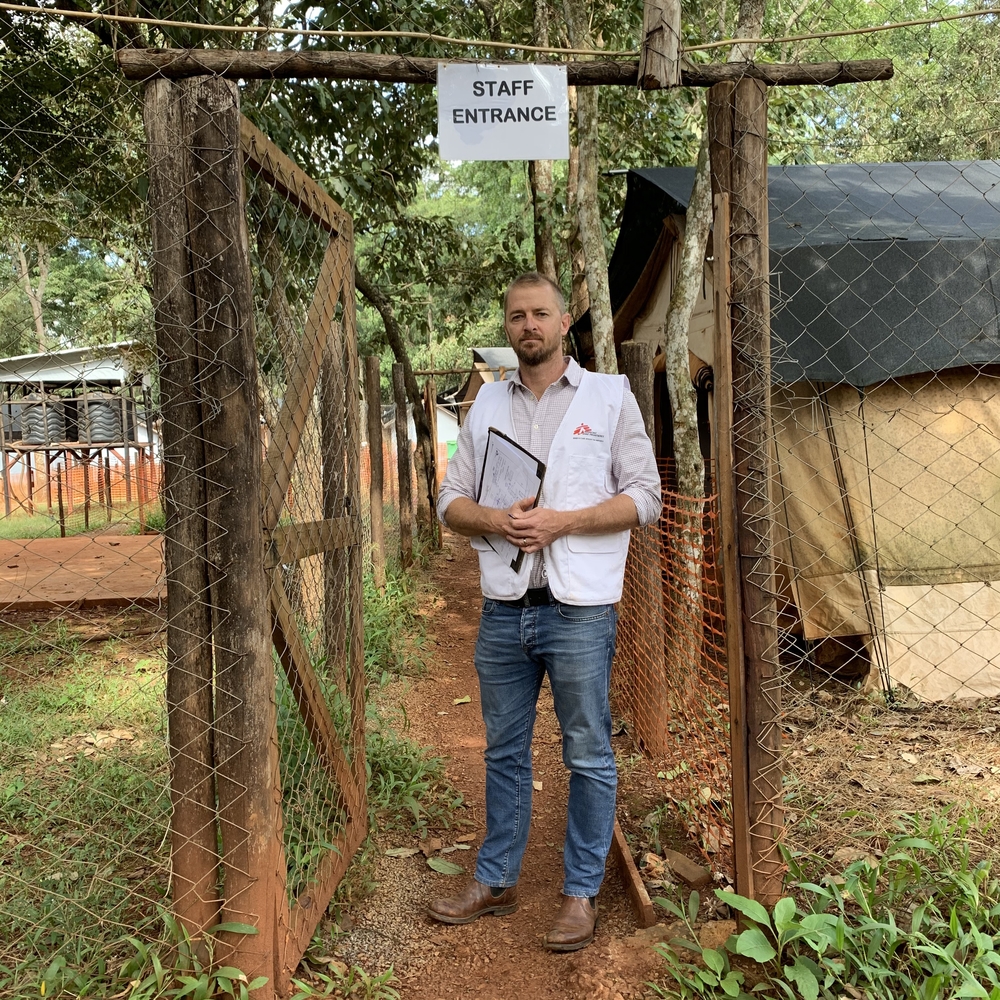
While the reported number of cases outside of China is relatively low, preparations to limit the further spread of SARS-CoV-2, the virus which causes the coronavirus disease (COVID-19), are essential. Dr Tankred Stoebe, MSF emergency coordinator, is currently travelling across Southeast Asia to assess how MSF can support health authorities and health facilities prepare for potential outbreaks of COVID-19. He describes his observations with a focus on patient vulnerability and simple control measures, which make a large difference.
Patient vulnerability
In countries where MSF is operational, our patients are of particular concern. It’s important to keep in mind that eight out of ten people infected with coronavirus only face a mild course or may not even notice it at all. Patients with already weakened immune systems however are likely to be more vulnerable to a severe course of coronavirus. We are already speaking to our patients, such as our Hepatitis C patients in Cambodia, what symptoms to look out for to in order to provide them with accurate information and to help alleviate their fears.
Simple control measues make a big difference
Lower middle-income countries like Cambodia or Laos have under-resourced health systems. They struggle to provide services to their populations even without the threat of a COVID-19 outbreak. If a major epidemic occurs, these health systems could collapse. Precautions and preparation are critical at this stage to avoid healthcare facilities contributing to the spread of the disease. I have seen that even simple disease control mechanisms are not yet in place. We are assessing the existing capabilities and might provide support to countries to develop their preparedness and response.
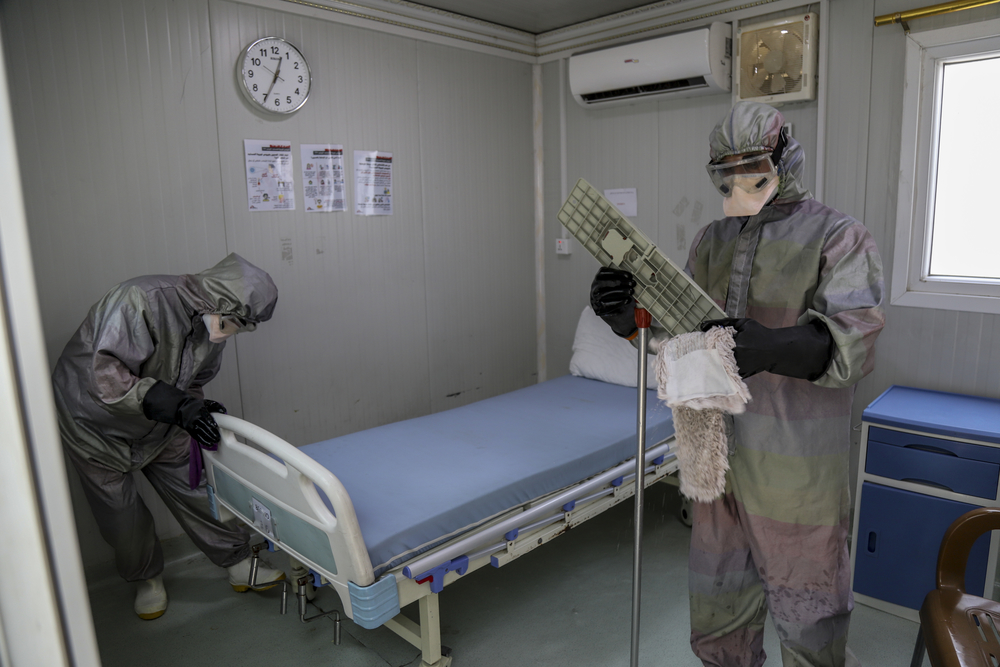
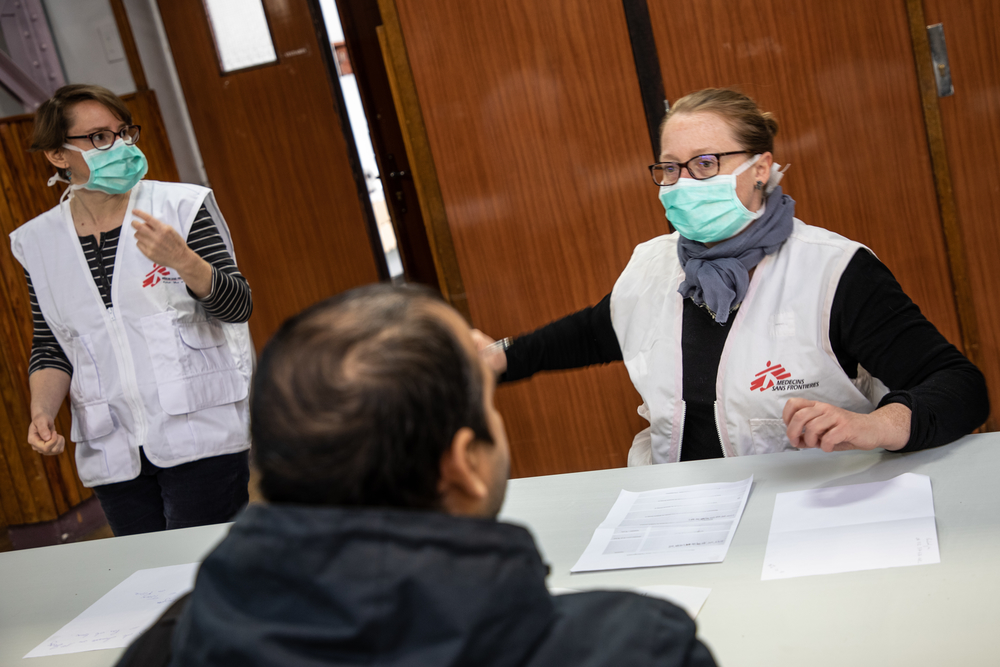
The most important step is to identify and separate suspected cases of coronavirus from other patients arriving to a hospital or any other health facility. You do this by establishing one entry point to a health facility in order to ask people arriving whether they have any symptoms. If they confirm having any symptoms, they should be taken to a separate, dedicated space to be tested and treated if the test confirms the infection. While this is a simple measure, the fact that it’s not in place shows that the health systems need support. I’ve attended a conference bringing together hospital staff for training on such precautions. We might need to work with the health authorities to implement training and put in place specific disease control measures within health facilities.
There’s a lot to be done and we need to use every minute we have to increase the preparedness to fend off an outbreak. I hope in the countries with fewer cases that the SARS-CoV-2 virus can be quickly contained. At the same time, I hope we can help other countries sufficiently prepare before the virus reaches their country.”