Ukraine: Four years of full-scale war
Three MSF staff share what it means to work, endure and care in wartime Ukraine.
“To be ‘alive’ is the lowest bar and the highest achievement for everyone”
MSF health promotion manager Katsa Juliana Shea joined MSF in January 2022 and has since worked in Bangladesh, Haiti and South Sudan.

“The absurdity of this war lies in its contradictions: the way life keeps going in parallel with the unbelievable destruction. There is the bravery and the sureness of the Ukrainian will, but also the grief, the fatigue of my friends and the weight of patients’ stories. There is the number of times you pass young men every single day, canes in hand and missing limbs. It’s impossible to get your mind around the scale and toll of it all. And yet, somehow, amid this absurdity — the alarms, the shelling, the drones menacing the sky — people still go to parks, children play and restaurants stay open. The horror and beauty coexist. You can’t help but carry that tension around with you like a small stone in your pocket, all day, every day, trying to understand how it can all be this way, how all of this fits together.
As you walk past the hundreds of beds side by side in an old school gymnasium, you see so many older couples in their 80s and 90s, sitting quietly under the dim lights, forced to finish out their lives in these extreme circumstances.
The shelling is at once terrifying and oddly banal. Your night is restless because of the scary hum of unmanned aerial vehicles followed by loud explosions that jerk you awake, not to mention the way your phone pings every few minutes with some air alert or security information. Yet the next morning, there’s this strange return-to-form, almost a defiance disguised as routine. As you walk to work the next morning, everyone you pass is tired like you. It’s written on all our faces. You feel a sort of solidarity with everyone knowing none of you has slept the night before and when you see your Ukrainian colleagues and ask them how they are, they will often say, ‘I’m alive.’ It’s not said in an ironic or even melodramatic way, it’s just the blunt, data-like truth of the situation. You realize ‘alive’ is both minimal and maximal, the lowest bar and the highest achievement now for everyone who lives in Ukraine.
These experiences reflect a broader reality faced by many. The frontline in Ukraine changes rapidly — recently by 10 kilometres in one night. As such, there’s been an increased influx of people arriving at evacuation centres set up some distance back from the frontline. As you walk past the hundreds of beds side by side in an old school gymnasium, you see so many older couples in their 80s and 90s, sitting quietly under the dim lights, forced to finish out their lives in these extreme circumstances. Recently, I spoke with one man who had walked kilometres to reach the evacuation centre with two dogs and two cats by his side. As we talked, he stood there with the dogs at his feet sleeping, the cat missing half its face. ‘These animals saved my life,’ he says. ‘There were drones above my head, but they didn’t attack me because they saw I had animals with me.’

The impact is uneven, filtered through different lives. The truth is, I feel it, but not in the same way as my dear friends and colleagues in Ukraine. I’m here, I’m under the same sky, I hear the same blasts, I see the same windows shake. I carry some of the adrenaline and some of the fatigue. But it’s not my brother on the frontline, not my house reduced to rubble, not my whole village and childhood, upbringing and family wealth erased. It’s not my history or my culture being fought for. There’s this constant doubling — where, on the one hand, I’m walking through it with them, drinking the same four cups of coffee the morning after, caring for the same patients and, on the other hand, I know there’s a kind of a barrier between their grief and mine, their risk and mine. Which leaves me feeling deeply part of this experience and also, very much outside of it — like I’m inhabiting someone else’s tragedy, but only as a guest, never with full ownership of the pain or the legacy of this war.


The fact is, there are so many stories that could just tear your heart out in the quiet moments of the day when you let yourself feel it, but sometimes it’s the deceitfully ordinary moments that really hit me, the ones that feel small until you realize they carry the weight of everything.
One afternoon, as I stepped out of my flat, I glanced upward and noticed my neighbours, this young and ridiculously cute couple, standing at their window. I waved and the man motions for me to wait. He disappeared briefly, then returned with the tiniest little newborn baby. He held the infant up to the window for me to see, beaming with such unguarded pride. I waved back. This image cements itself into my mind: a family, living under drones circling above, so deserving of peace. It’s just one of the countless small miracles that persist. My friend told me the Ukrainian phrase ‘бути у надії’ used to say someone is pregnant, literally translates to ‘be in hope.’ For sure, this hope, this investment in the future, is the resilience carried forward.”
“We have been surviving the coldest winter Ukraine has experienced for years”
Robin Meldrum has been in Ukraine since 2024, working as a country director on projects mainly based in the east, close to the frontline.

“Is the situation in Ukraine worrying and frightening and deeply depressing? Spoiler: It is and it seems to be getting worse.
It was around this time that we had an incident in the frontline city of Kherson, in the hospital where we have an embedded medical team. The city is attacked on a daily basis with hundreds of artillery shells and short-range quadcopter attack drones. That day there was particularly widespread artillery shelling throughout the city and several mortar rounds landed in the hospital compound. Fortunately, none of the buildings were directly hit. Our team is well drilled in how to react and they go to the safe basement shelter whenever there is an increased risk. I went to the hospital the following week to meet the director.
His reaction will be forever etched in my memory. His tension when he thought we were meeting to say we would no longer be able to work in that hospital was clear from the moment we walked in the door. And his relief when we said we intended to stay was palpable. He explained he would struggle to maintain the emergency department and intensive care units of the hospital without MSF’s additional support, and said the idea the MSF team would leave had been worrying him for the past week.
We all know why we are here. There are people in very vulnerable situations that need medical care and they deserve all our efforts. And each passing week the needs grow as the machine of war grinds on.
This is what we see everywhere we go along the 600 kilometres or so of near-frontline areas where MSF teams are working. Hospitals and primary healthcare centres are struggling to cope with enormously depleted staff numbers. One general hospital we were supporting near the frontline in the east had no surgeon until the MSF team proposed to embed a medical team. During 12 months, our team performed or assisted 452 surgeries in this hospital, until the frontline got too close and we had to withdraw and start supporting another hospital a bit further back from the active combat area.
The patients we treat and transport by ambulance are an indicator of how civilians are impacted. Pretty much every village you go to in the 50-kilometre zone from the frontlines has some civilians who have remained. They are usually older people who have lived there all their lives, not wealthy and with deep anxiety about leaving – where will they go? What will they do for food and shelter? What will happen to their home while they are gone? Many of these people have chronic medical conditions and the primary healthcare options that they would normally rely on have been reduced or sometimes completely disappeared. We try to reach as many of these communities as possible with mobile clinics, but our hospital teams see far too many older adults arriving in a critically sick condition, after missing out on their regular treatment plans for hypertension, diabetes or other conditions that ought to be easily manageable. The average age of patients admitted into the intensive care unit we support in Kherson is 63 and many are much older. They often arrive in a critically urgent condition and sometimes too late.


Over the past two months, we have been surviving a very difficult winter, the coldest Ukraine has experienced for several years. Russian attacks have been targeting electricity and heating infrastructure and the consequences have been brutal. I had to move into a colleague’s apartment after a month with no running water, no flushing toilet, very intermittent heating and sometimes only two or three hours of electricity per day. I would often wake up in a room that was three or four degrees Celsius, which is the recommended temperature inside a fridge. Many of my Ukrainian colleagues have had the same experience, having to leave their homes to move in with friends or colleagues, because when temperatures drop to 20 degrees sub-zero, just surviving becomes a struggle if you have no heating.
A potential attack is never more than 10 or 15 minutes away and this threat is ever-present, 24 hours a day, seven days a week. Everybody has their own ways of coping. I try to appreciate little moments of beauty and normality. The rooks circling and calling at sunset over the Dnipro river in Kyiv, while the imposing 300-foot-tall statue of ‘Mother Ukraine’ fixes an indomitable stare over the river to the east; the two lesser-spotted woodpeckers that would come every morning to the old walnut tree outside our house in Mykolaiv; good chats with friends over a beer or coffee in one of the many excellent bars or cafes in Kyiv or Dnipro; a memorable summer barbeque on the sandy beach on the shore of the Pivdenny Buh river in Mykolaiv (I copied some of the locals and went for a quick swim and it was lovely).

But above all, I find motivation and inspiration in our 320 Ukrainian colleagues. They have endured this for four years and the energy-sapping fatigue is clear. Some, who originally come from the eastern region of Ukraine, have lived this war for 10 years now. Nobody I know is free of mental and emotional scars. But the determination and commitment they show, every day, arriving in the morning mustering all their energy to do their job as well as possible – it is an extraordinary source of inspiration.
We all know why we are here. There are people in very vulnerable situations that need medical care and they deserve all our efforts. And each passing week the needs grow as the machine of war grinds on.”
“I have met patients whose courage and determination deeply impressed me.”
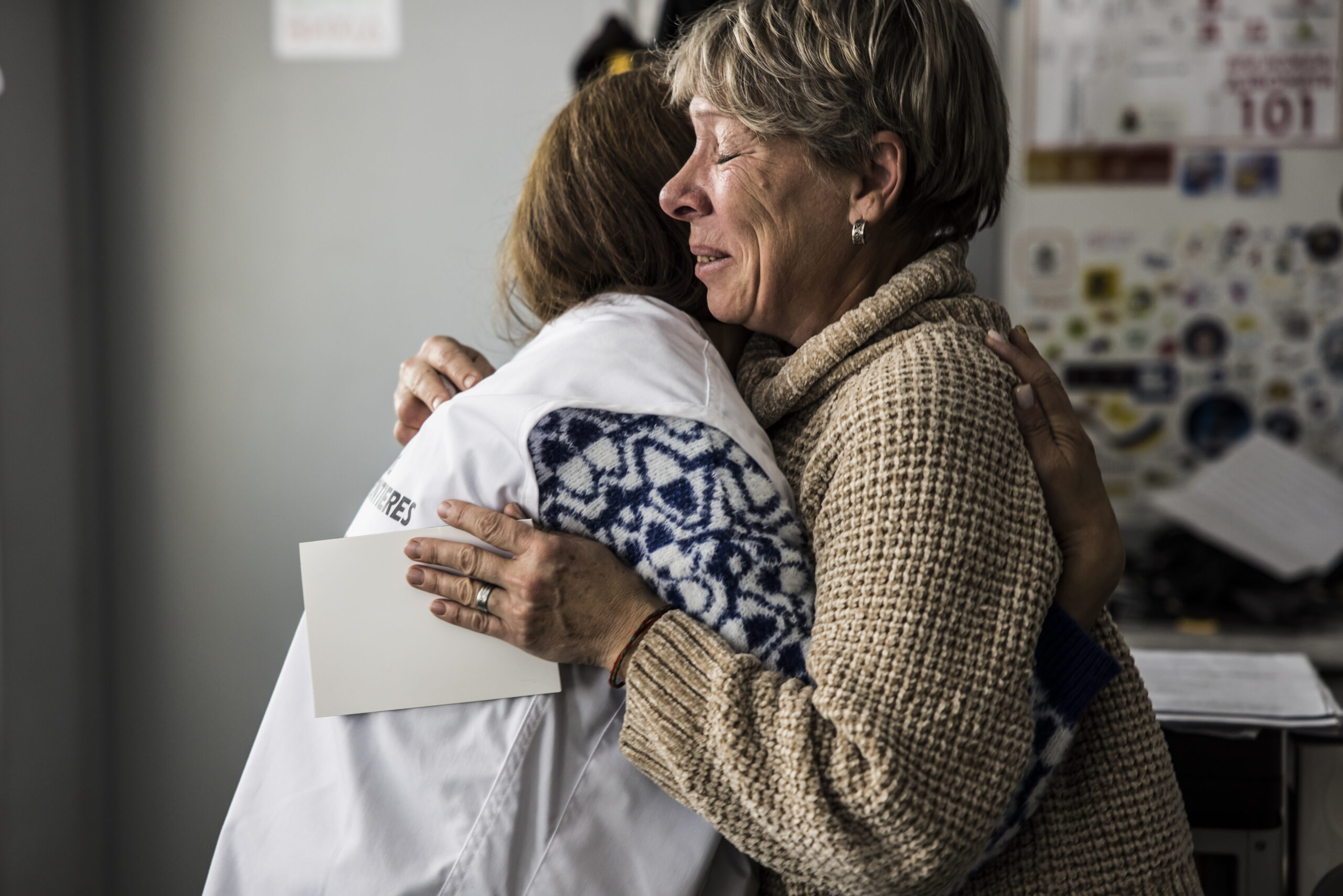
MSF medical coordinator Christine Mwongera. She has with the team at the Vidnovlennia healthre centre in Vinnytsia, where we provide psychological counselling and treatment for people experiencing symptoms of war-related post-traumatic stress disorder (PTSD).

“For the past two and a half years, I have been working in Ukraine, supporting people affected by the war. My impression of the international armed conflict here is it has deeply disrupted people’s lives —their families, their homes— and has taken away their sense of safety. This winter has felt particularly intense compared to the two previous winters I spent in Ukraine. Russian forces have systematically targeted energy, heating and water infrastructure with missiles and drones during periods of severe frost. The cold and unpredictable electricity have made daily life feel heavier and have required constant adjustments. This includes creating ways how to stay warm inside the apartment that’s around seven degrees Celsius, or finding ways to adapt to the light schedule (some days there may only be two hours of light per day). Many people have suffered from the harsh winter and power shortages — I feel it myself, I hear it from my colleagues and I see it across Kyiv.
But people in Ukraine are truly remarkable. I’ve seen incredible solidarity in how people organize themselves to support one another and keep going, despite the difficult times. Through MSF’s Vidnovlennia mental health centre in Vinnytsia, where we support people who have experienced trauma, I have met patients whose courage and determination deeply impressed me. I remember individuals who had been through extremely difficult experiences — losing their homes, losing family members, being forced to relocate — yet they spoke about their families, their neighbours and their future plans for themselves and their children. The hope they carried has stayed with me for a long time.
I am Kenyan, and when I first arrived in Ukraine I found the social distance between people noticeable. Kenyans tend to be very expressive and quick to socialize, while Ukrainians seemed reserved at first. But once they opened up to me, the connection was sincere and meaningful — especially now, when they know you share the experience of war. And I do share that experience.

I am often based in Kyiv and like many residents of the capital I experience nights of heavy attacks on the city and its energy infrastructure. Monitoring channels such as phone application and telegram channels often warn of incoming shelling. There are certain safety rules to follow, such as going to shelters or following the ‘two walls’ rule, there should be at least two solid walls between you and the street. This means the ‘safest’ places are the bathroom, hallway, closet or dressing room. Those nights can feel very long. Even after it becomes quiet, the body still holds tension and fear about what could have happened — mixed with the relief of being safe. One habit I have developed to cope after shelling is to limit news consumption and focus on positive thoughts. Sleep is often disrupted and it can take time to recover and return to a normal routine.
I have always wanted to work where people need support the most. For me, this work is meaningful. Even the smallest action we take can have a real impact on someone at a very difficult moment in their life.”