Access to Medicines
Doctors Without Borders/Médecins Sans Frontières (MSF) continually calls on governments, pharmaceutical companies, researchers, and others to place lives before profits and commit to making essential medicines available and accessible to the patients around the world who need them most.
As a humanitarian medical organization driven by the belief that everyone should have access to essential health services, MSF provides critical medical care, free of charge.
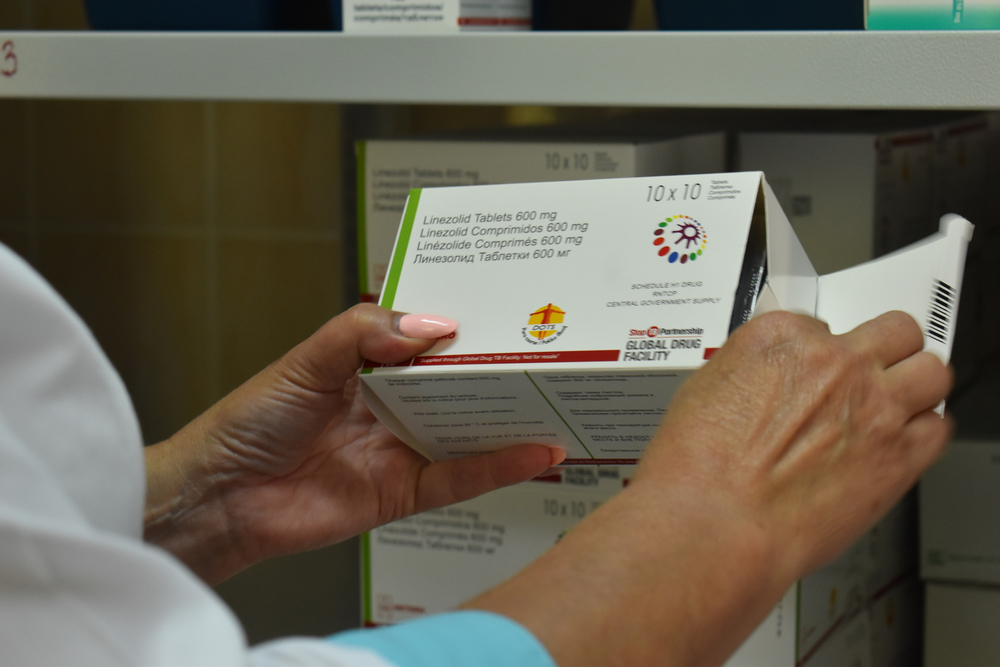
Too often, however, our teams cannot treat patients because the medicines they need are too expensive, not available or have never even been developed to treat some of the diseases we encounter. Sometimes, the only drugs we have are highly toxic or ineffective, and nobody is developing a better treatment.
Bringing down prices, stimulating research
That is why in 1999 we started the Campaign for Access to Essential Medicines – now known as the Access Campaign – to help overcome the many barriers that prevent people from getting the treatment they need to stay alive and healthy. The Access Campaign focuses on bringing down prices and ensuring medicines are available in countries that need them, and on stimulating research into improved treatment options.
As a provider of emergency humanitarian medical care to people affected by crisis and conflict, MSF finds it fundamentally unacceptable that access to vital medicines is increasingly difficult for patients and health systems in the places where we work, including for common and infectious diseases, because of a pharmaceutical development and supply system driven by the logic of commerce rather than public health needs.
Unfortunately, the global medical supply system is not set up to respond to pressing public health needs in places with limited resources. Instead, it is mostly driven by the interests of the for-profit pharmaceutical industry. As a result, the health priorities of MSF’s patients and their communities are rarely shared by pharmaceutical companies, often because the medical needs of lower-income countries and at-risk global populations are not considered profitable enough to invest in.
As a result of this system of profit-before-public health, millions of people around the world face life-threatening health risks for which effective medicines are not available. There is a critical need for new drugs and health technologies that can meet their needs.
Why it matters to Canadians
We believe small Canadian steps – in medical research and development funding, in research prioritization and in biomanufacturing – can have a big impact on the ability of patients around the world, and in Canada itself, to access essential medicines when they need them most. That’s why MSF is calling for Canada to reassess its priorities and to place lives ahead of profits when it comes to publicly funded health innovations.
Every year, Canada’s government invests millions of dollars in health innovation, whether through the government’s own labs or in support of Canada’s medical research and development sector and publicly funded universities. This level of public investment makes possible the creation of new medical technologies guided by public health needs rather than profit motives.
The problem is that Canada doesn’t actually demand these investments of public funds result in affordable or accessible medicines, vaccines or other health technologies, whether in Canada or around the world. In fact, the medical innovations Canada funds are most often licensed or simply sold off to private companies, with no strings attached.
That means even when Canada has shouldered the risk and financial burden of developing new medicines or other health technologies, they still become the property of private companies. Those companies are then free to charge high prices as they see fit, even for medicines that can make the difference between life and death.
Canada can do better with public funds
MSF and its supporters are demanding Canada attach common-sense conditions to the funding it provides for medical research and development. Recipients must be required to ensure medicines and vaccines developed with public funds will be affordable, available and accessible to people who need them most.
Without immediate action to attach such safeguards, the Canadian government risks spending millions to develop new medicines controlled by private pharmaceutical companies and priced out of reach of patients and health systems — including Canada’s.
Canada is home to many world-class medical researchers, many of whom focus on diseases for which effective treatments, diagnostics and other medical technologies either do not already exist or are in need of significant improvement. These include diseases that MSF teams confront on a regular basis in many of the places where we work, such as Lassa fever, cryptococcal meningitis (a leading cause of death for many people infected with HIV) or visceral leishmaniasis (kala azar). With the right amount of support – and a research and development model based on producing public-health value rather than profits – Canadian researchers can produce the medicines and health technologies patients need.
And while getting these kinds of innovations out of the lab and into the clinics where they’re needed most would once have been difficult without the involvement of large, profit-seeking pharmaceutical companies, here too Canada has an opportunity to show how things can be done differently. Recent government investments in publicly funded biomanufacturing facilities can help secure medical supplies for Canada itself in the event of future pandemics But they can also focus on areas of unmet global need by ensuring publicly funded pharmaceutical infrastructure is dedicated to public health needs, rather than facilitating private profits.