MSF tells MPs that Canada must do more to address inequitable global access to vaccines
The following is a transcript of opening words by Jason Nickerson, Doctors Without Borders/Médecins Sans Frontières (MSF) Humanitarian Representative to Canada to the Canadian Parliamentary Standing Committee on International Trade in May 2021.
Hello, thank you for having us.
We’re going to speak to two issues that are part of the Committee’s study, from the perspective of our organization which provides medical assistance to people affected by crises in more than 70 countries around the world.
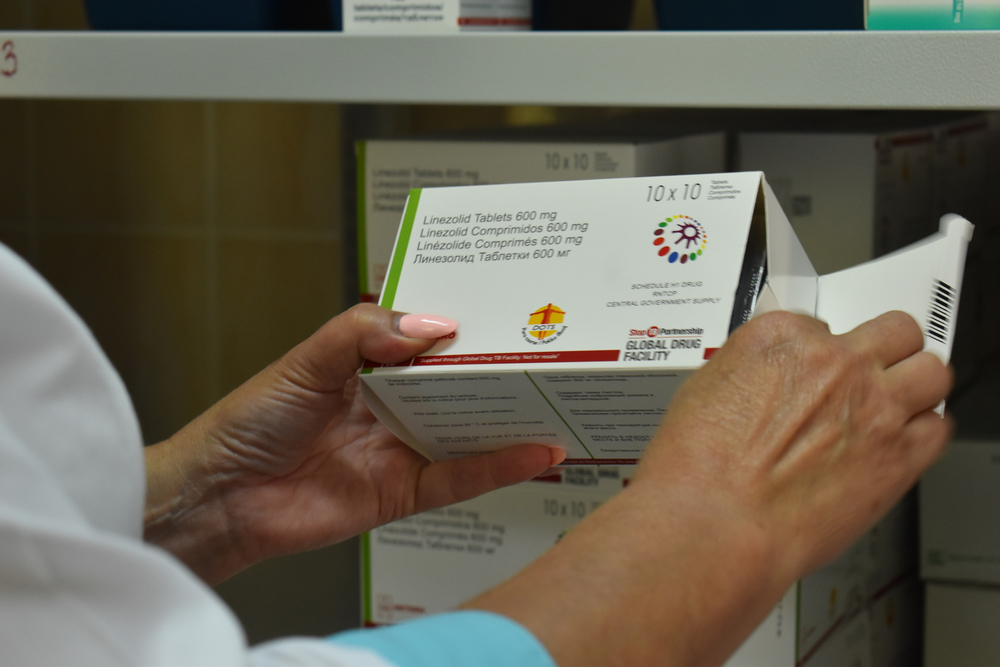
First, Canada should support the TRIPS waiver. The waiver is not a complete solution to scaling-up and diversifying COVID-19 vaccine manufacturing to address the supply shortages, but supporting the waiver, and quickly, clears space and removes legal barriers to focus on the many other barriers. We emphasize that any waiver must encompass not only vaccines but other tools, like therapeutic drugs, diagnostics, and medical devices like ventilators as well as components and equipment needed to make vaccines.
Canada’s position during the discussions around the TRIPS Waiver has been one of indecision – never formally rejecting it, while repeatedly raising alternatives that have failed in the past. One such alternative raised is the TRIPS Article 31bis mechanism, which is operationalized by Canada’s Access to Medicines Regime, or CAMR. It is our position that Canada should follow through on its own claims of CAMR’s effectiveness by taking the necessary first step of adding COVID-19 vaccines and drugs to Schedule 1 of the Patent Act. While MSF does not believe that TRIPS Article 31bis or CAMR are effective tools at the best of times, let alone sufficient in this pandemic, Canada’s failure to even list these items in Schedule 1 means Canada is the single greatest roadblock to utilizing the very tools it has promoted at the WTO.
The second issue we would like to discuss is domestic production. MSF supports increased domestic production, but it must be done correctly. If Canada’s approach to scaling-up biomanufacturing in this country is to provide financial support to pharmaceutical companies to build factories here, this funding must come with guarantees of affordable access to the final products both for Canada and the rest of the world. This is just common-sense: if the public is paying to develop and manufacture medicines, we should all be able to access them at fair prices. To this end, Canada must also be transparent about the terms of all such deals.
Another key question is what to do between pandemics with the public manufacturing capacity Canada is building. New quality-assured manufacturing capacity that’s been initiated for the purposes of producing COVID-19 vaccines should not be shut down or sold off to private interests after the pandemic fades. Rather, Canada should use this capacity to address other important global health issues. Producing a range of products keeps facilities operating and Canada’s skills sharp – after all, it’s not clear what the next pandemic will be and the world needs a diversity of manufacturing capacities.
Canada has world-class researchers. Where it falls short is end-to-end development to get innovations out of labs and to patients. Products that are vital for global health, but have limited commercial appeal, have no real pathway to approval. Take the Canadian-invented Ebola vaccine, discovered by scientists at the National Microbiology Laboratory in Winnipeg. After discovering it, Canada signed a deal to license it to an American company. This ultimately led to the vaccine languishing on a shelf for years; this meant this effective vaccine was not ready in time for the 2014 west African Ebola outbreak. To be blunt: This cost lives. Canada has other promising experimental vaccines, like for Lassa fever and Marburg virus that have faced similar challenges. End-to-end production, from lab bench to patient bedside, ought to be part of our biomanufacturing strategy.
Our overarching message here is that there are many important diseases that are essentially market failures – they are not profitable enough to attract investment from private pharmaceutical companies, yet represent significant public health threats. Ebola, Lassa fever, Marburg, and prior to this pandemic – coronaviruses – are all examples. There are also many important drugs and vaccines that already exist that are regularly in shortage or hard to obtain. Diphtheria antitoxin – the product Connaught Labs was founded to produce – is now almost impossible to procure worldwide. We know this first-hand as when we were responding to simultaneous diphtheria outbreaks in Yemen, Bangladesh, and Venezuela in 2017, we quickly realized how few options existed. The same is true for many antibiotics and other low-profit medicines.
A robust biomanufacturing strategy that is guided by public health needs, and not the pursuit of profits, is what needs to guide Canada’s biomanufacturing strategy, which ought to be linked to an R&D strategy. We have experts in open science collaborations who are prepared to do this here, and we have models of innovation that can prepare us for future pandemics. This is no time for business as usual, it’s time for Canada to regain some of our global health leadership that’s been squandered during this pandemic, by being a net source of vital drugs and vaccines for the world. Thank you.