COVID-19: MSF launches it’s largest ever response in Belgium
With just over 1,000 deaths from COVID-19 recorded for a population of 11 million, Belgium is one of the countries hardest hit by the pandemic, coming close behind Italy and Spain. Despite Belgium’s highly developed health system, Doctors Without Borders/Médecins Sans Frontières (MSF) has launched its largest ever response in the country to support key areas including infection control in hospitals, care for the elderly and support for vulnerable groups such as homeless people and undocumented migrants.
Belgium – like a number of other European countries – is facing a very intense phase of the COVID-19 pandemic. Every single day of the past week, close to 600 people were admitted to hospital, while more than 1,000 patients are currently in intensive care. Although just half of the country’s dedicated COVID-19 hospital beds are full, some key gaps in services exist, prompting MSF to launch its response.
Bringing MSF’s outbreak response expertise to hospitals
One might assume that with one of the most advanced health systems in the world, Belgium would not need an organization like MSF to help it cope with a health crisis. But despite its many hospitals providing quality care and its large numbers of medical staff, Belgium is simply not used to facing major outbreak situations.
“Hospitals in Belgium don’t need MSF to provide quality care,” says Meinie Nicolai, MSF’s general director. “But what we do bring is our expertise – developed responding to cholera, Ebola and plague – on how to organize a hospital and how to organize the flow of patients to prevent further infections, so that people can be treated in the best possible conditions.”
MSF teams have already started work in hospitals in two of the worst affected areas: Mons and Antwerp.
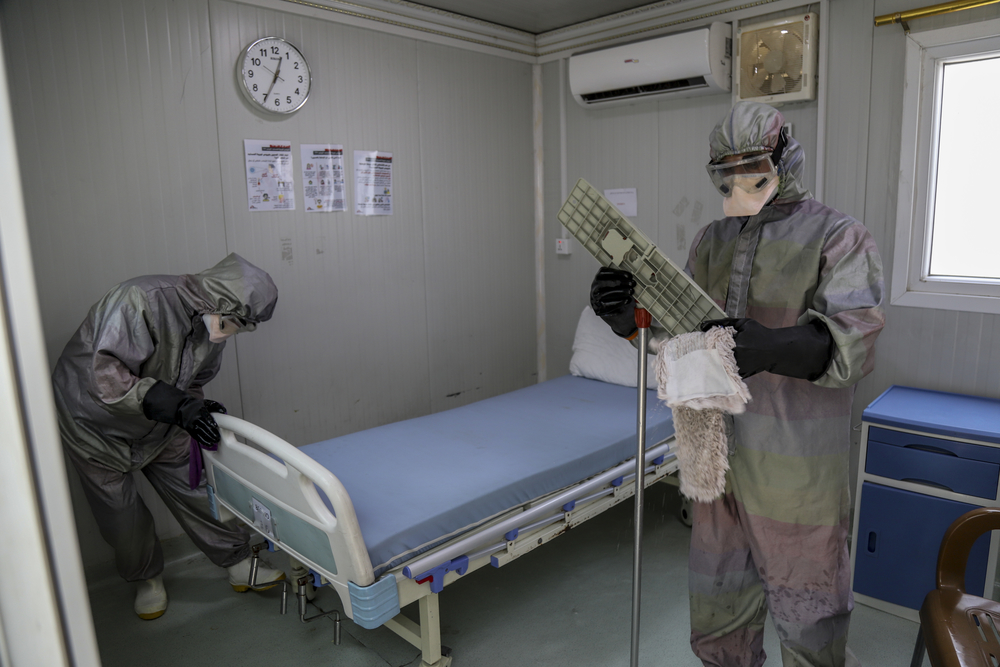
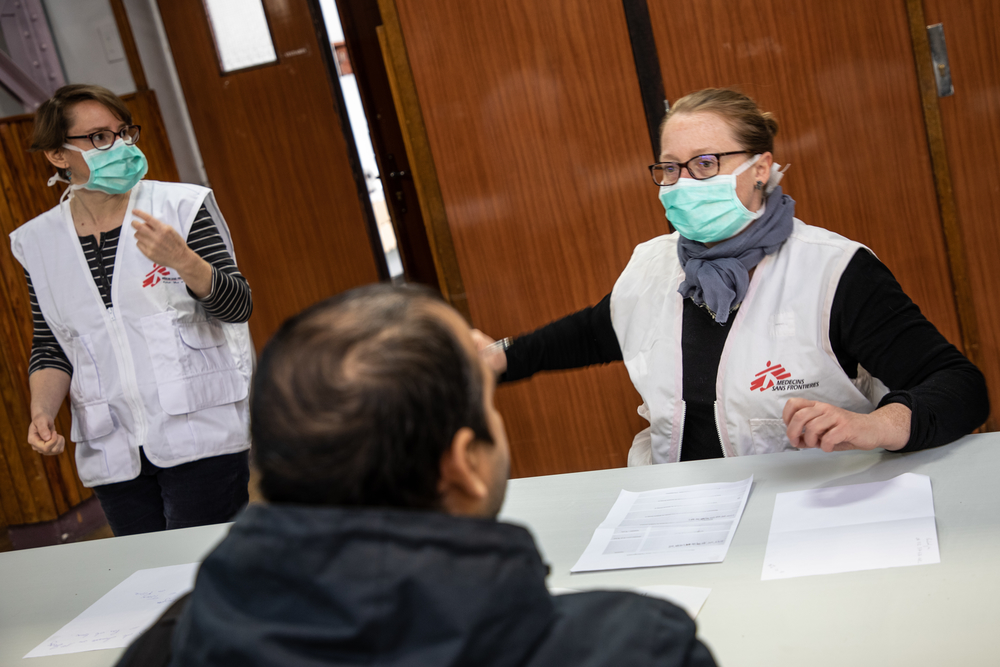
In the Centre Hospitalier Universitaire Ambroise Paré in Mons, an MSF team of five medics and three logisticians are providing medical support and training in the use of personal protective equipment (PPE) and infection control measures, including how to work safely when there is a shortage of protective equipment.
The MSF team is also helping the hospital employ better separation between COVID-19 patients and other patients, and advising on how the hospital’s capacity and function could be adapted in response to various scenarios. The team will also provide psychological support for the hospital’s medical teams, who have been working extremely hard in very difficult circumstances for some weeks.
“When we arrived, there was a large number of patients, and the numbers are increasing every day,” says Stephan Goetghebuer, MSF’s COVID-19 coordinator in Mons. “Our collaboration with the hospital has been very fruitful, and we and they are learning how best to adapt to the situation. We hope that this experience of working in a hospital heavily impacted by the outbreak, combined with our experience in many other epidemics, will allow us to provide rapid support to other hospitals in the worst affected areas of the country.”
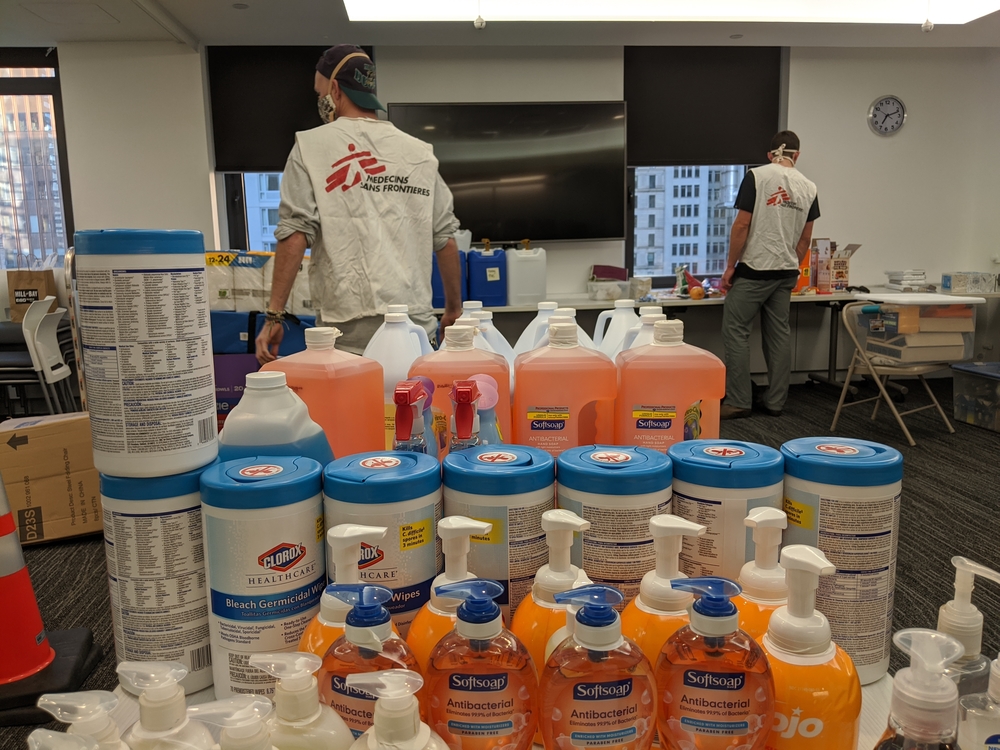
In Antwerp, MSF has set up ‘washing zones’ in the Stuyvenberg, Middelheim and Jan Palfijn hospitals where protective aprons worn by health staff caring for COVID-19 patients can be properly cleaned and disinfected. MSF is also providing support and training in infection control measures and PPE protocols at all three hospitals.
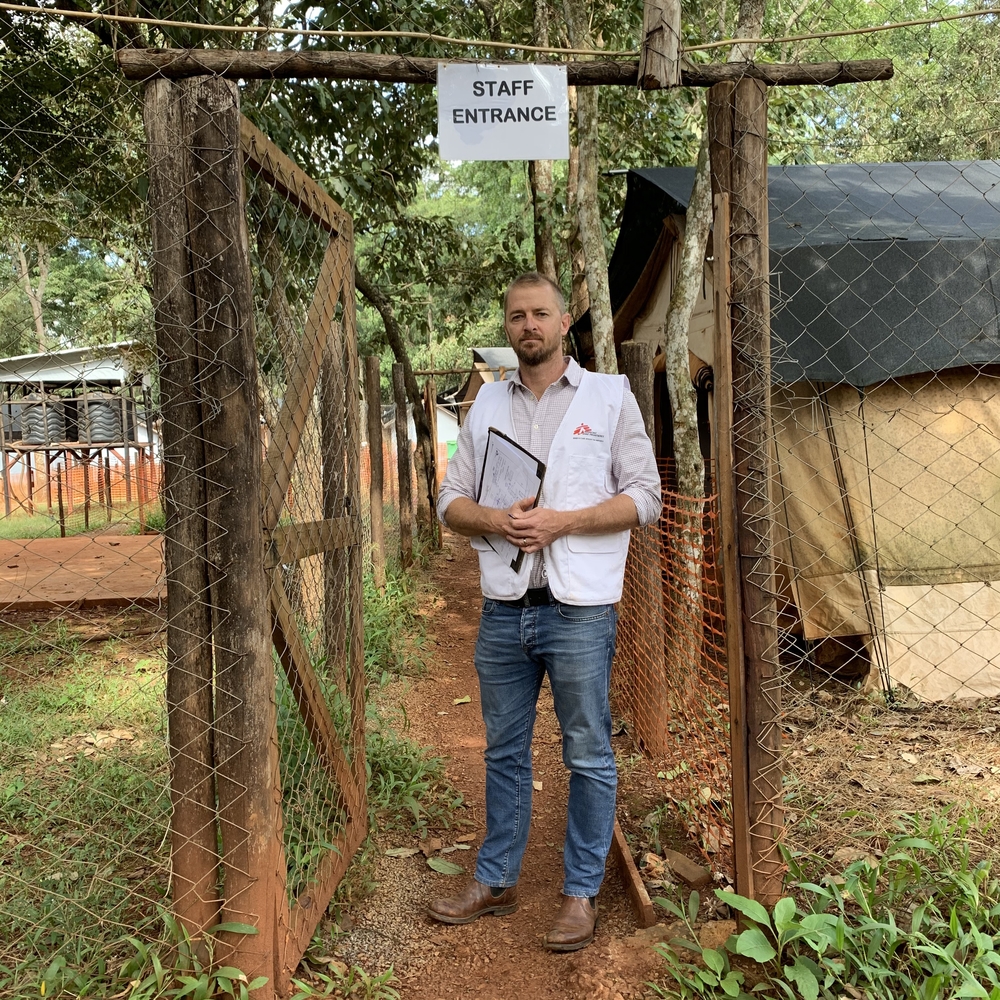
In Antwerp and Brasschaat, MSF teams are providing support to local authorities as they set up dedicated health units for COVID-19 patients, including technical support in protective measures and health management.
In Lier and Sint Truiden, MSF teams are providing support to two health units, one with 20 beds and the other with 40 beds, where recovering COVID-19 patients who no longer need intensive care are cared for by medical staff before returning home.
MSF plans to document its approach regarding hospitals and health units so that it can be replicated elsewhere without the need for direct support by MSF teams.
Care for the elderly
As in the rest of the world, the novel coronavirus kills disproportionately among the eldest in our communities, with more than 93 percent of COVID-19-related deaths in Belgium occurring among the over-65s. For the elderly, the double blow is that many medical staff are so overloaded with work that they cannot cope with the demand to visit care homes. In response to this gap, MSF is sending mobile teams of nurses and health promotion professionals to visit more than 150 care homes in Brussels. During their visits, the teams check if any residents are infected with the virus, organize the best way to isolate them from other residents, and arrange for the best possible medical care in the absence of regular visits by doctors.
The mobile teams also support and train care home staff in how to disinfect potentially contaminated areas and on how to use protective equipment most effectively when it is in short supply.
Supporting the most vulnerable communities
Unfortunately, many people in Belgium live on the streets – a situation made worse by the closure, due to COVID-19, of a number of centres for homeless people and undocumented migrants. Ordinarily, people with symptoms are recommended to self-isolate at home, which is obviously impossible for people who have no home to go to. In response, MSF has opened a centre where rough sleepers who have tested positive for COVID-19 can stay and receive medical care, and from where they can be referred to hospital if their symptoms worsen. The 50-bed centre can be extendable to 150 beds if needed.
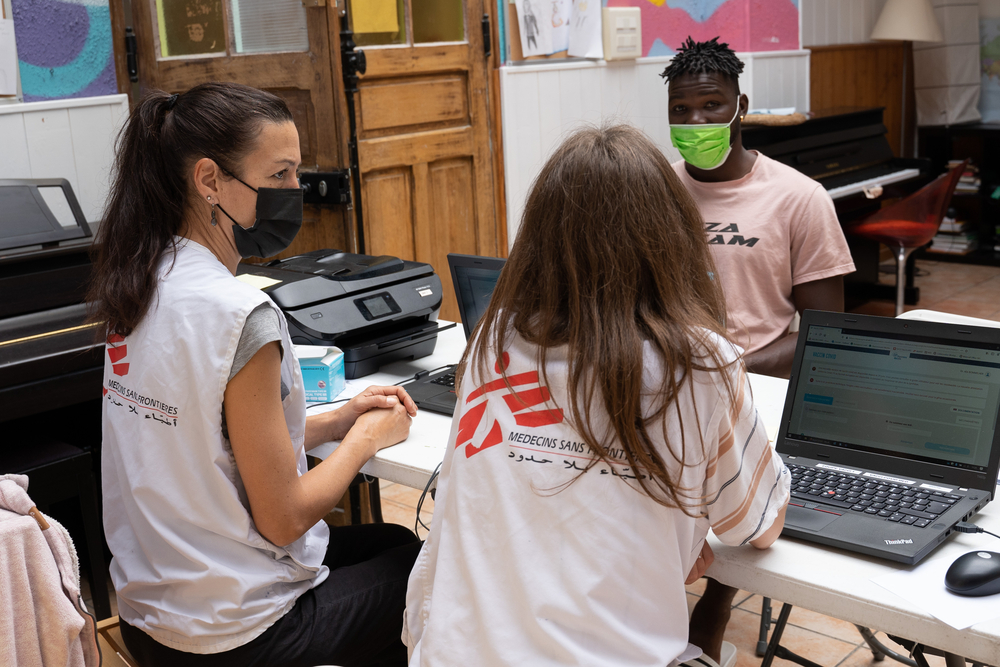
An MSF team is continuing to do COVID-19 triage and referrals in the Humanitarian Hub in Brussels, a place where MSF and six other organizations provide care to migrants and asylum seekers all through the year.
Many challenges ahead
With 115 staff deployed in total, MSF’s response in these key areas in Belgium should help – but will obviously not replace – the tremendous work done by all medical staff since the beginning of the outbreak. Health workers across the country are facing various challenges, including shortages of protective equipment such as aprons and masks, while many more challenges lie ahead.
“Medical staff and all frontline workers in Belgium should be more systematically tested so that hospitals and health centres do not themselves become hotspots of new infection,” says Meinie Nicolai. “Vulnerable groups – like the elderly, the homeless and undocumented migrants – should also be more systematically tested so that we can break less visible chains of transmission and so that they can get proper care.”