MSF opens Khayelitsha Field Hospital as South Africa braces for COVID-19
In May, South Africa’s Health Minister warned that with the current infection rate, South Africa would surpass its hospital bed capacity, potentially by the end of June.
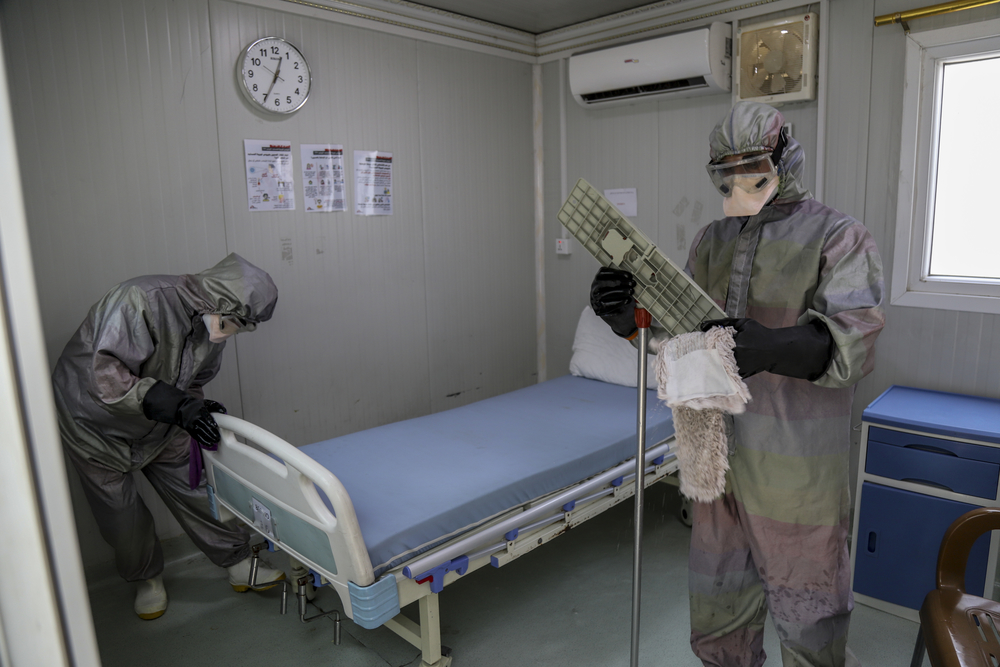
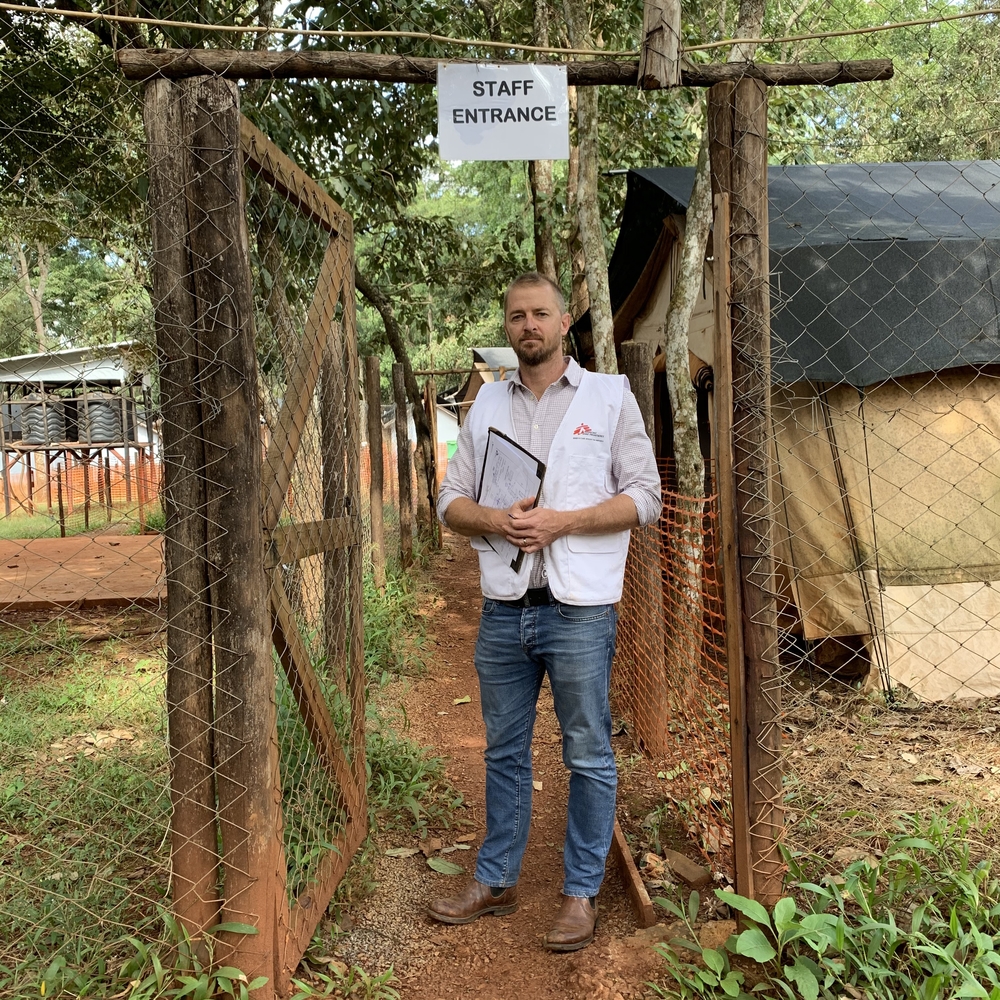
“As COVID-19 continues to spread, the wards in Khayelitsha District Hospital have filled up with suspected and confirmed cases. We are helping increase local healthcare capacity to meet these urgent needs – this will help save lives,” explains Dr Eric Goemaere, project leader of a COVID-19 Field Hospital developed by Doctors Without Borders/Médecins Sans Frontières (MSF) in Khayelitsha Township, a densely populated settlement within Cape Town.
The Khayelitsha community has borne the brunt of COVID-19 infections in the country, spurring MSF to develop the 60-bed overflow treatment facility, which will manage moderate to severe COVID-19 patients in support of the local hospital.
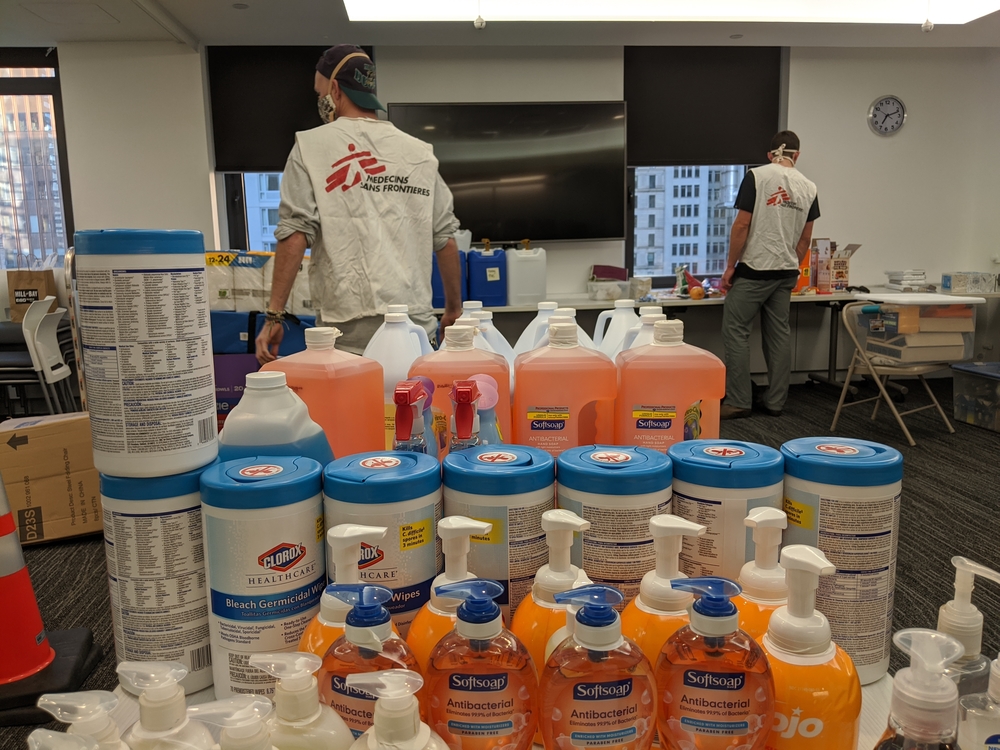
“Given that patients will be suffering from respiratory distress, all beds will ultimately be equipped with oxygen concentrators,” Goemaere explains
MSF opened the Khayletisha Field Hospital on June 1st, in the presence of the National Minister of Health. A day later, the facility received 24 COVID-19 patients from the local hospital.
Where COVID-19 Hits Hardest
Khayelitsha was the first township in South Africa to record a confirmed COVID-19 case, in late March, and has since been the community worst hit. Over half of Khayelitsha’s estimated 500,000 residents live crowded together, in shacks and informal housing. Unemployment sits at 42% of the population, and 60% of residents lack running water in their homes. Amidst the extreme poverty, COVID-19 infections have risen from around 25 infections daily in May, to over 150 daily infections in June – an alarming 600% increase.
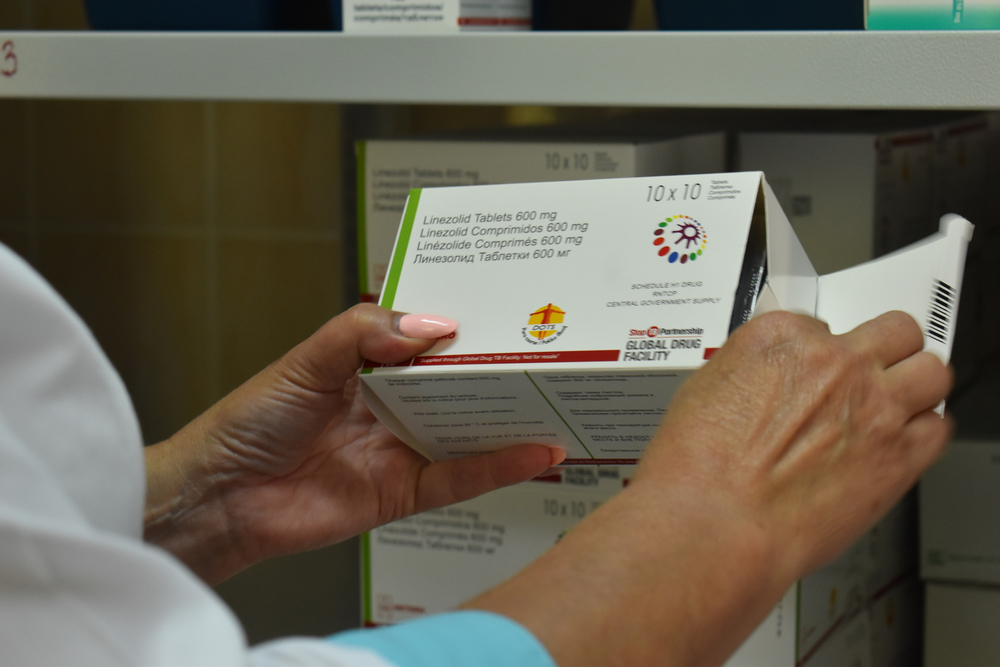
Maintaining Care for HIV/TB Patients
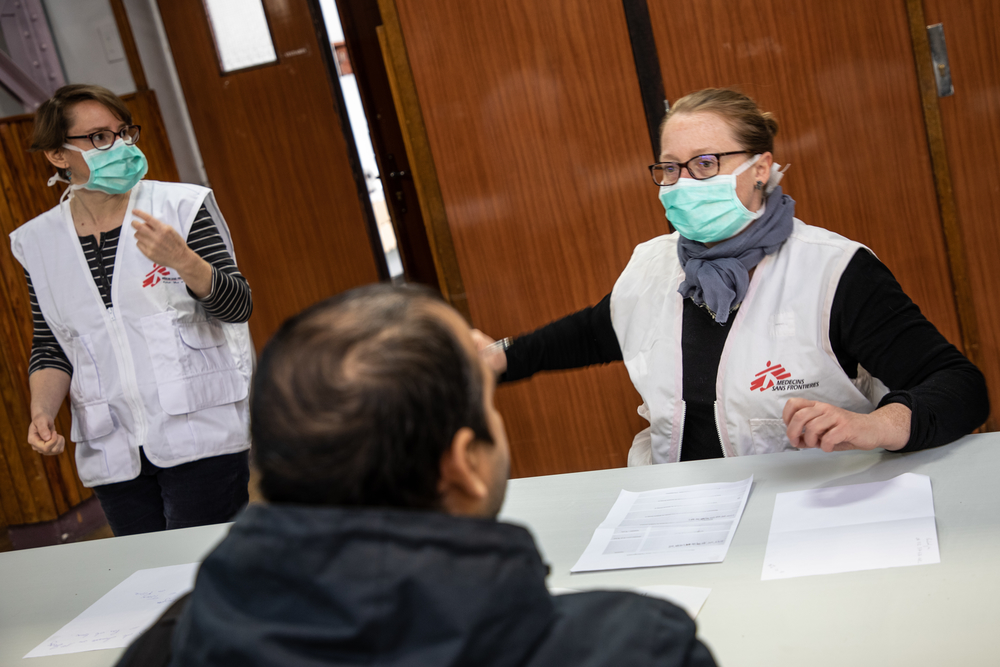
“We are here to help cope with a major humanitarian emergency. But we are not just talking about COVID-19. We are working to provide treatment for COVID-19 while maintaining our services for people with two of the most prevalent chronic diseases, HIV and tuberculosis (TB),” explains Nompumelelo Zokufa, a Health Promotion Manager with MSF in Khayelitsha.
MSF has worked in the Khayelitsha community for over 20 years, developing innovative strategies for care at all stages of the treatment process for people living with HIV and/or drug-resistant TB. As the health system becomes overwhelmed by COVID-19, HIV and TB programs have been disrupted. Restriction of movement to reduce the spread fo COVID, in addition to patients being afraid to leave their homes to pick up their medicine from clinics, or even get tested due to the risk of coronavirus infection, means that fewer people visit health centers. It’s also likely that many of those who arrive at healthcare facilities with TB are misidentified as COVID-19 suspects, as the symptoms are similar.
“The more we learn about COVID-19, the better we can adjust our response. We now see that essential healthcare, including HIV and TB services, have been negatively impacted across the board,” explains Dr Laura Trivino, MSF medical coordinator in South Africa.
Adapting to the Challenges of COVID-19
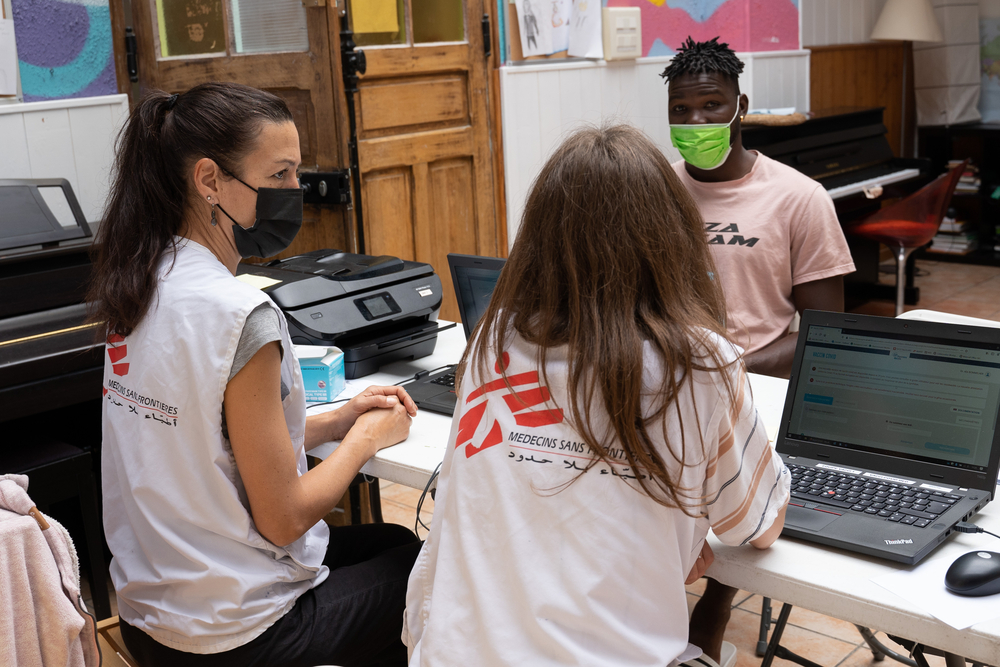
South Africa’s Department of Health, with the help of MSF and other partners, has been attempting to find a balance between addressing COVID-19 while ensuring that HIV and TB are not forgotten.
“The COVID-19 response aims to separate people, especially those at high risk from severe COVID-19 disease, from the risks, and one way of doing this is to move certain services outside of health centers, which are potential infection hotspots. In practice, MSF has been helping local authorities to give HIV and TB patients longer medicine refills, even supporting the delivery of medicines to their homes. We also supported screening for COVID-19 at facilities as a way of preventing those with COVID-19 from infecting other clinic-goers,” Trivino says.
But in order to prevent COVID-19 measures from completely disrupting HIV and TB services, it is important that HIV and TB testing is quickly and effectively integrated into the COVID-19 response.
“We have been supporting the Department of Health to do this, because we can’t afford to lose the ground we’ve gained over the last years on HIV and TB. We are all learning together, applying our past experiences in dealing with epidemics, and ensuring that the community is always at the centre of everything we do,” Trivino says.