COVID-19 vaccines: Equitable global access is urgently needed
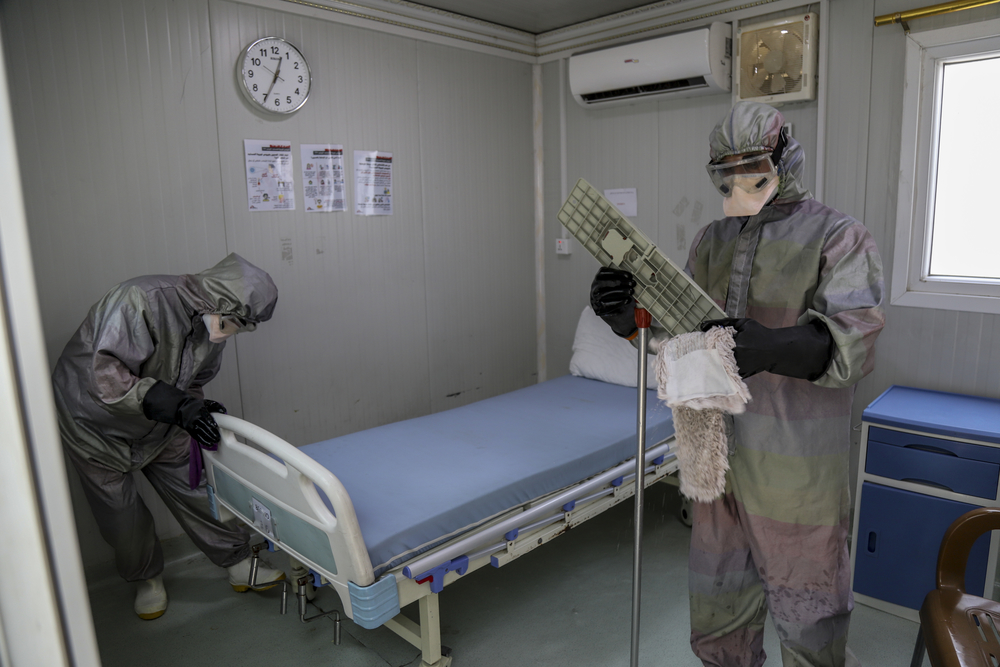
COVID-19 is a devastating global public health emergency, especially in parts of the world where healthcare systems were already fragile even before the pandemic began. The key to overcoming this disease is through vaccination.
The rapid development of multiple COVID-19 vaccines has been an unprecedented and remarkable achievement. But we are already seeing how global access to them is deeply inequitable. Access is being determined not according to levels of public health risk but according to wealth.
Leaving low-income countries behind puts everyone at higher risk
Rich countries that can afford them are buying up most of the available global supply of vaccines. Low-income countries, which are unable to pay the same high prices, cannot compete. They have been forced to the back of the line, unable in many cases to vaccinate even their front-line health workers, and dependent on still-unclear plans for charitable vaccine donations from others.
This is no way to respond to a global pandemic.
Distributing vaccines according to the commercial interests of the pharmaceutical companies that make them — companies that have already received billions of dollars in funding from governments around the world — is a flawed approach that will leave the virus to spread relatively unchecked through countries unable to access the vaccines they need.
It is not only inequitable, it’s bad public health: As the virus spreads, it will continue to evolve, making it more likely the world will face new variants against which our current vaccines will no longer be as effective.
MSF is calling for equitable global access to COVID-19 vaccines
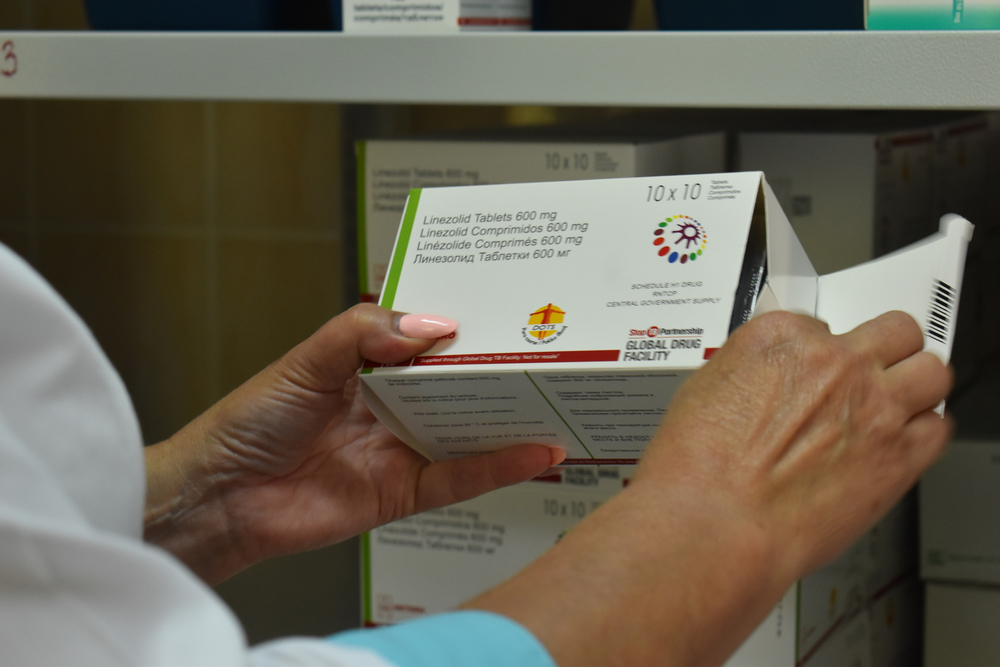
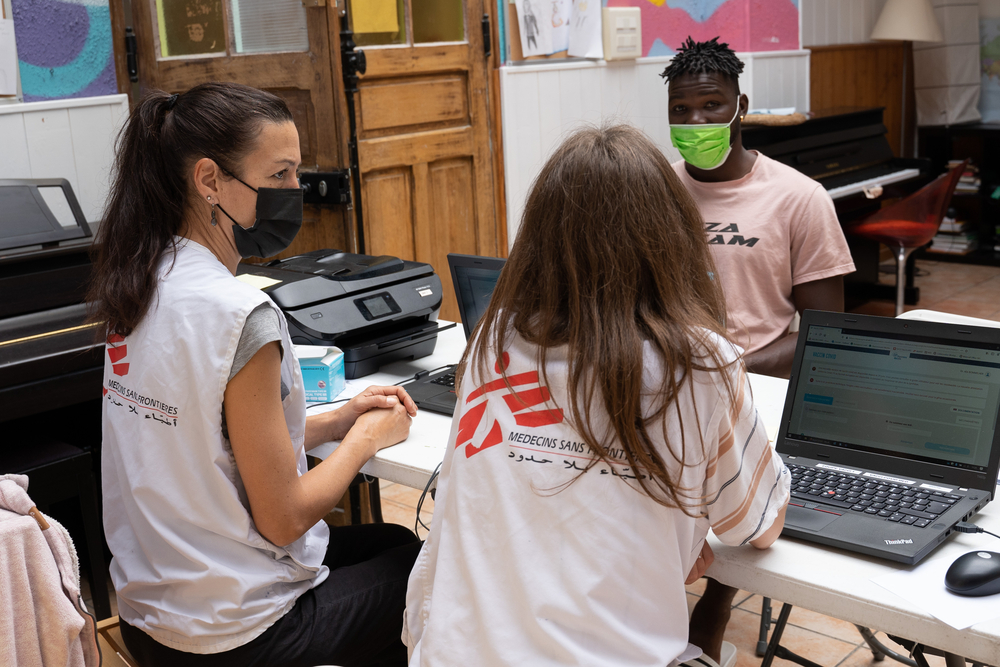
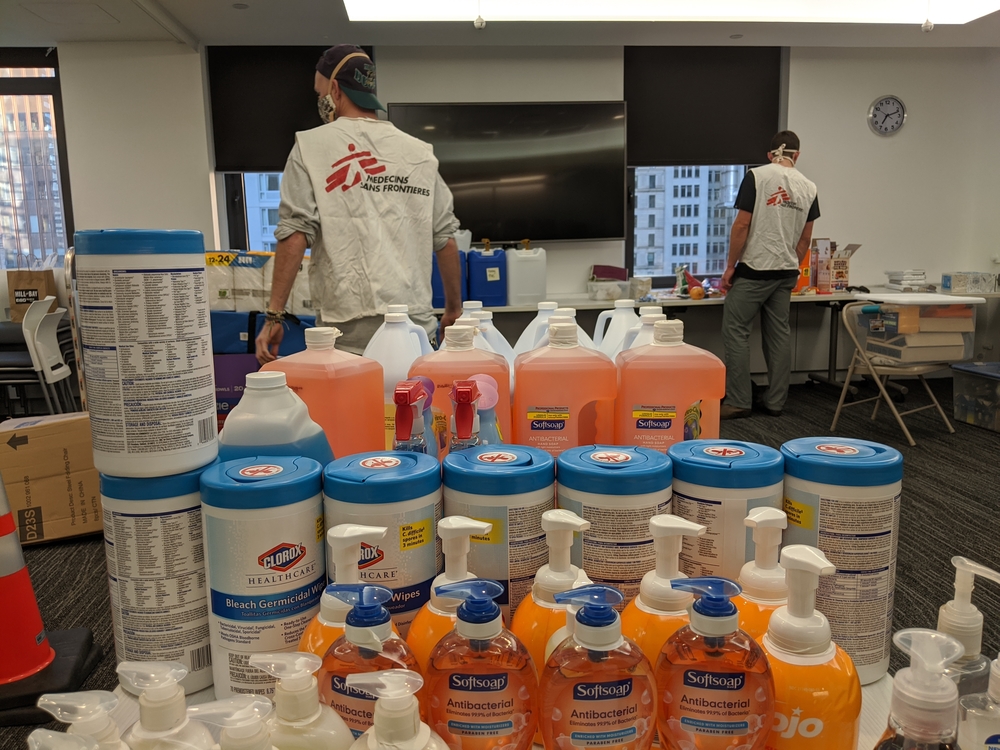
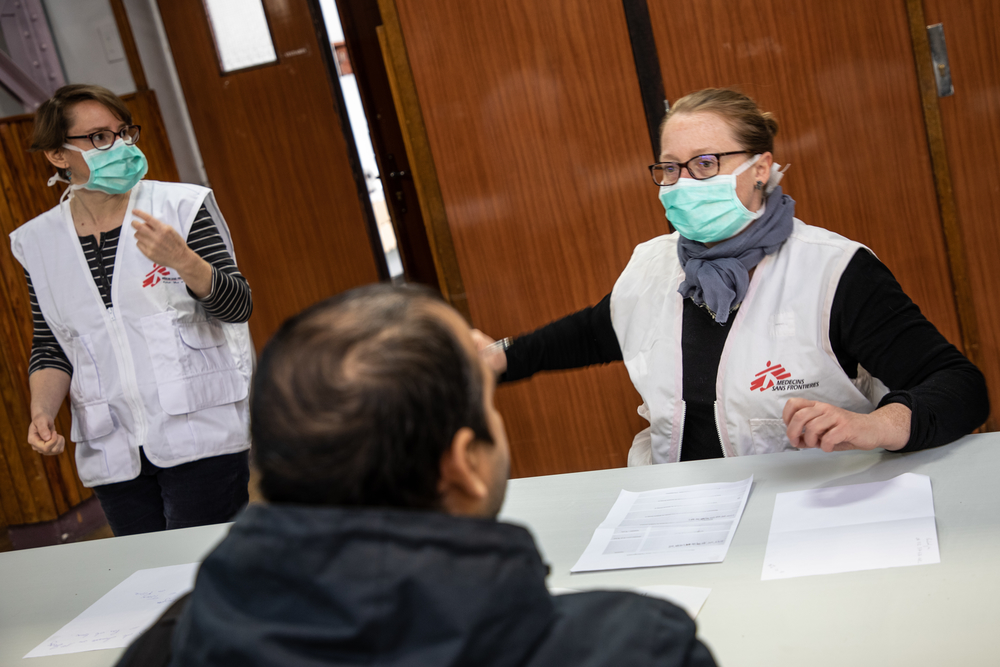
Doctors Without Borders/Médecins Sans Frontières (MSF) has been calling attention to global disparities in access to medicines for decades. We have seen first-hand how even urgent health needs around the world are frequently left unmet in places too poor to be considered profitable markets by pharmaceutical companies.
When it comes to COVID-19, that is not just morally unacceptable, it’s bad for global public health.
There is no global plan to ensure everyone has access to a vaccine
The problem is no plan exists to make sure all countries will have access to the vaccines they need.
That’s because the commercial logic of the current global pharmaceutical system treats vaccines — even for a pandemic that won’t be over anywhere until it’s over everywhere — not as essential public goods, but as commodities that can only be distributed through private sales or donations.
But this business-as-usual approach will not protect the world’s most vulnerable people, nor help to end this pandemic. That’s why MSF is calling for a different approach to vaccine distribution, one that prioritizes the greatest number of lives saved over the greatest amount of profits made.

Who is getting all the COVID-19 vaccines?
The rollout of COVID-19 vaccines has given rise to many questions from the public to governments across the world.
Who is getting a vaccine first? Who is supplying the vaccines? How long will it take until everyone is vaccinated?
Right now, most of the world’s available supply of COVID-19 vaccines is going to a relatively small group of wealthier countries, who have been able to make their own bilateral purchase agreements with vaccine manufacturers — usually at prices that remain undisclosed.
Canada, for its part, has signed deals to buy enough doses to vaccinate its entire population five times over. Despite a slow start to receiving those doses, Canada is on track to vaccinate everyone in this country who wants to be vaccinated by fall 2021.
Much of the rest of the world will not be so lucky.
By the end of 2021, for example, any countries depending entirely on the COVAX facility — the global mechanism developed to help middle- and low-income countries access COVID-19 vaccines — are forecast to have only received enough doses to vaccinate less than seven per cent of their populations.
Even when the full COVAX distribution program is eventually rolled out, it will only cover 20 per cent of targeted populations, and there is no clear plan yet in place for how the rest will receive any vaccines at all. Current expectations for many countries are that sufficient coverage will not be possible until at least 2023.
That means many of the highest-risk people in low-income countries will likely not receive a vaccine until well after the lowest-risk people in high-income countries. This is unacceptable.
The COVAX Facility: How Canada helped low-income countries negotiate better access to vaccines – and then competed against them
The primary global effort to address inequitable access to COVID-19 vaccines is the COVAX Facility, an initiative in which both high-income and low-income countries have pooled together as a single large purchaser, allowing available doses to be allocated at the same time for all countries according to what is needed to vaccinate everyone’s highest-risk populations.
Canada was an early and significant supporter of COVAX, and is also a participant — an important commitment to making this initiative viable, since the facility depends on the participation of wealthier countries.
However, COVAX has struggled to acquire enough funding and enough doses to meet its first target of covering just three per cent of participating countries’ populations in the first half of 2021 — in part because countries like Canada, in addition to participating in COVAX, have also gone ahead with their own private bilateral purchase agreements, competing directly against COVAX and undermining the whole principle of equitable access to vaccines in the process.
Right now, COVAX is one of the only ways for many low-income countries to acquire the COVID-19 vaccines they need. It is essential that it be enabled to work properly, that it be sufficiently funded, and that wealthier countries with their own purchase agreements do not further impede supply to those countries who are depending on COVAX.
More information about Canada’s role in COVID-19 vaccine and COVAX:
- MSF Q&A: Canada and the COVAX Facility
- MSF responds to news of first deliveries of COVID-19 vaccines through the COVAX Facility
No patents in a pandemic: Intellectual property, the World Trade Organization and the People’s Vaccine
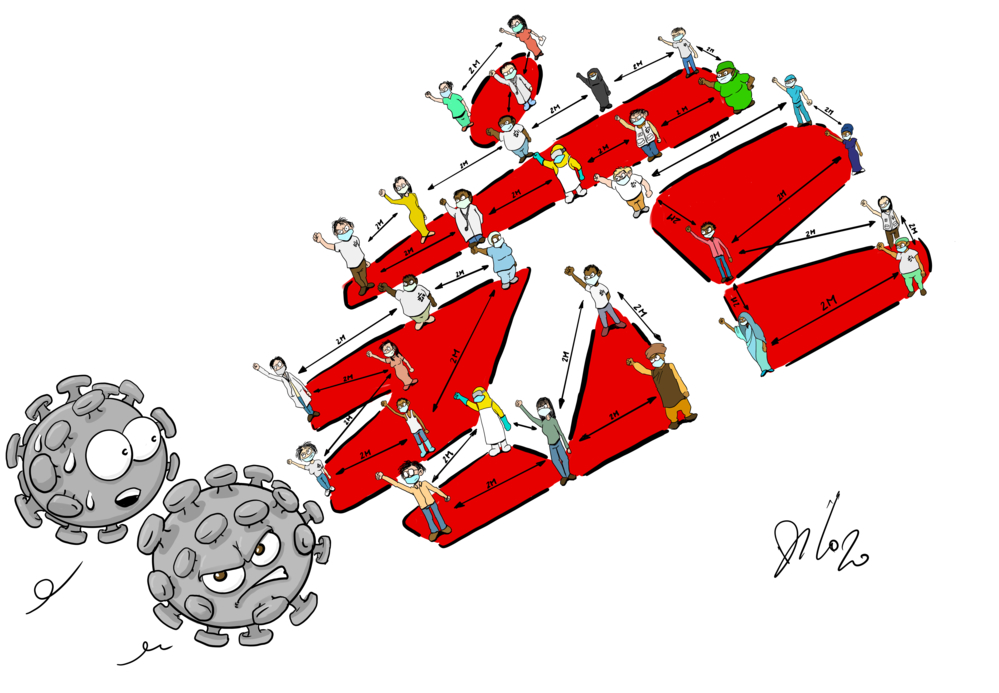
Ending the COVID-19 pandemic globally will require mobilizing and upgrading production capacity everywhere to ensure a maximum number of doses can be manufactured and equitably distributed at the lowest possible price — for everyone around the world, including Canadians.
This requires pharmaceutical companies to share technology, know-how, biological material, and intellectual property with other qualified producers, and to do so quickly.
Companies such as Moderna, Pfizer, BioNTech, AstraZeneca, Novavax and Johnson & Johnson — who are leading in COVID-19 vaccine production, and have also received billions of dollars in public funding from governments around the world to develop those vaccines — face a choice: either defend their monopoly power and deny hundreds of millions of people rapid access to these lifesaving vaccines, or commit to a People’s Vaccine by increasing access, supply and affordability for COVID-19 vaccines for all people in all countries.
MSF and the #NoCovidMonopolies waiver proposal at the World Trade Organization:
Last October, India and South Africa proposed a waiver at the World Trade Organization (WTO) on intellectual property rights for all newly developed health technologies related to COVID-19 for the duration of the pandemic. This would allow countries to choose not to enforce, apply or implement patents that impede the production and supply of COVID-19 vaccines, drugs and other medical tools. If adopted, the waiver would send a crucial signal to potential manufacturers that they can start producing needed COVID-19 medical tools without fear of being blocked by patents or other monopolies.
But while more than 100 WTO member countries support the proposal, a small number of countries — including Canada and others who have already secured the vaccine doses they need for their populations — are obstructing it. MSF is calling on them to drop their opposition, and for the waiver proposal to be accepted as quickly as possible.
- Why Canada should not block the TRIPS waiver at the WTO: An MSF Canada briefing paper
- 5 reasons a new proposal by India and South Africa could be a gamechanger in the COVID-19 response
- Countries must stop blocking and move toward formal negotiations on pandemic monopoly waiver at WTO
Lives Over Profits: How Canada can take action against vaccine inequity
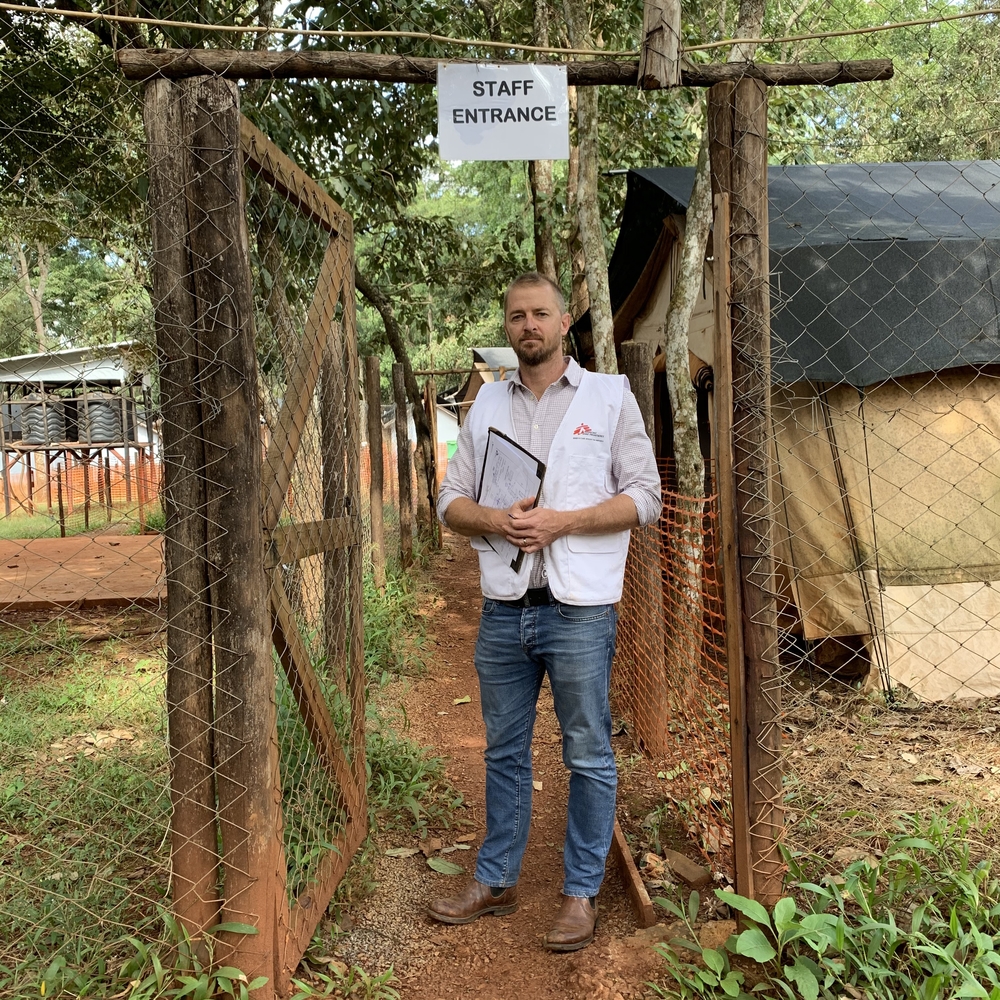
Recently, MSF was asked to speak directly to Canadian parliamentarians about the global risks and impacts of COVID-19 one year into the pandemic. Dr. Jason Nickerson, MSF Canada’s Humanitarian Affairs Advisor, addressed members of the House of Commons Standing Committee on Health by saying:
“If we fail at equitable distribution of COVID-19 vaccines, we fail at global public health. It’s that simple. This would be morally catastrophic and a significant risk to the public health of all people, including Canadians.”
Jason Nickerson | MSF Canada Humanitarian Affairs Advisor
TWEET THIS:
What makes such a failure — already evident in the struggles of the COVAX Facility to access enough doses for its participants — distressingly likely to occur are the inherent flaws of our current system for the development and distribution of essential medicines. “I want to emphasize,” Dr. Nickerson told the committee, “that the only reason for COVAX’s existence in the first place is because the way the world currently develops, manufactures, and delivers new medicines and vaccines is broken. It is set up to maximize profits. The pharmaceutical industry is not set up to rapidly respond to emerging pathogens with pandemic potential, it is not designed to scale up manufacturing of new health technologies to meet global demand, and as we are seeing today, and have seen for decades, it is not set up to ensure equitable access to new medicines and vaccines, particularly for people in economically poor countries.”
What can Canada do about that?
MSF offered three recommendations to the Health Committee:
1. A public timeline for Canada to make its surplus doses of COVID-19 vaccines available for use in low-income countries to vaccinate healthcare workers and other high-risk people.
2. Making the funding Canada provides to develop new medicines and vaccines conditional on those outcomes being made available to people around the world at affordable, fair prices.
3. Requesting that the Parliamentary Budget Officer review any drugs and vaccines that have been discovered and developed with Canadian public funding to understand whether under a different model of production we might have more affordable and accessible options for public health needs, both in Canada and around the world.
Public medical R&D funding in Canada: An opportunity for change
At the heart of these recommendations is the fact that, every year, Canada’s government invests millions of dollars in health innovation, whether through the government’s own labs or in support of Canada’s medical R&D sector. In 2020, Canada’s government spent more than $1 billion on research related to COVID-19 alone. This level of public investment makes possible the creation of new health technologies guided by public health needs rather than profit motives.
The problem is Canada currently does nearly nothing to ensure these investments of public funds result in publicly accessible outcomes. In fact, the medical innovations that Canada funds are most often licensed or simply sold off to private companies — with no strings attached.
That’s why MSF and its supporters — including the more than 91,000 Canadians who signed our petition ‘Lives Over Profits’ to the Canadian government last year — are demanding Canada attach conditions to the funding it provides for medical R&D, requiring recipients to ensure medicines and vaccines developed with public funds will be affordable, available and accessible to those who need them most.
This is how Canada can start to make a real difference and help establish critical medicines such as COVID-19 vaccines as essential public goods, not privately held assets.