Responding to COVID-19 in Myanmar: A letter from the team on the ground
Myanmar’s public healthcare system is in disarray. Days after the military seized power on February 1, 2021, medical staff walked out of their jobs, spearheading the civil disobedience movement that saw government employees of all stripes go on strike. Most have not returned. Those on strike who continue to practice in underground clinics risk being attacked and detained by the authorities. At least 28 healthcare professionals have been killed since February 1, 2021, and nearly 90 remain arrested.
When Myanmar’s beleaguered public healthcare system met with a far-reaching and devastating COVID-19 outbreak, hospitals were quickly overwhelmed.
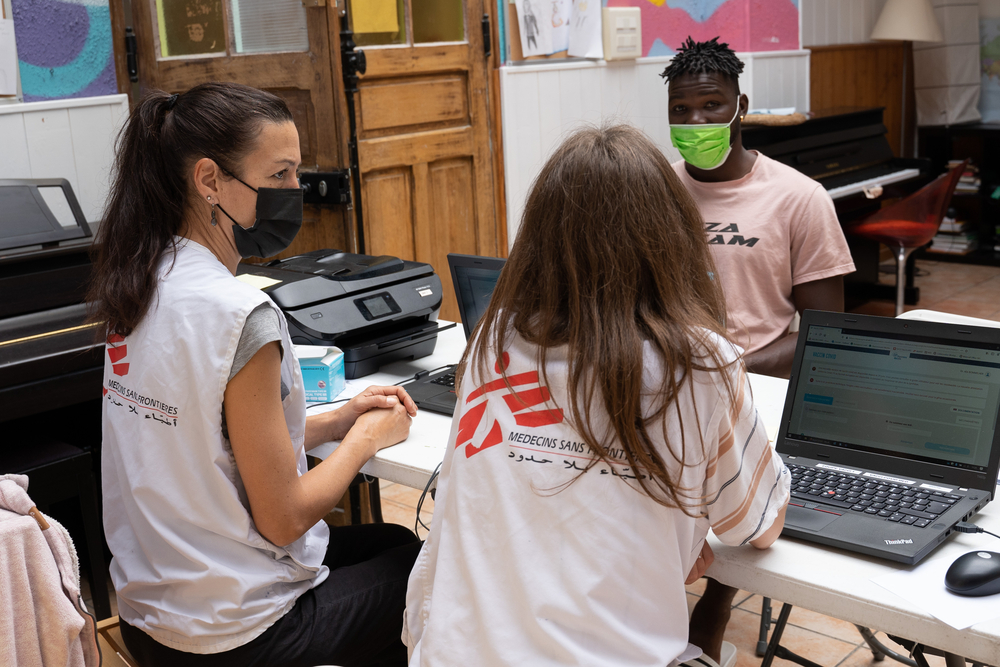
With 2021 about to come to an end, we, as the Doctors Without Borders/Médecins Sans Frontières (MSF) team in Myanmar, are looking back at our COVID-19 response, reflecting on what we can be proud of and what we could have done better; the dilemmas, limits and the sometimes-uncomfortable solutions.
Overcrowded crematoriums and empty shelves
As COVID-19 infections peaked, beds in hospitals were often impossible to come by and untold numbers of people were scrambling around towns and cities in Myanmar to source their own supplies of oxygen to administer at home.
Crematoriums could not process the bodies fast enough. Routine consultations, surgeries and vaccinations were cancelled while the skeleton medical workforce responded to the outbreak. Panic buying led to empty shelves in pharmacies.
Naung Ting, a 34-year-old caregiver at our treatment centre in Myitkyina, Kachin state, told us how when his father-in-law fell ill with COVID-19, he could neither get admitted to the local hospital where he lived in Danuphyu, Ayeyarwaddy region or in Yangon two hours away.

“At that time, my relatives who are doctors in America made a messenger group and they were giving remote treatment for him. It meant we had to buy medicine on our own. We had to arrange the oxygen and the cylinders,” he said. “Relatives who had no medical experience of giving injections had to do it. And the medicine was so expensive.”
Demand pushed up the price of a drug to treat blood clots, which are common among COVID-19 patients, to 40,000 kyats (US$22) a pill. He had to take two every day. Naung’s family could only find one oxygen cylinder, and they needed to travel to Yangon and back every other day to refill it. Ultimately, his father-in-law could not get enough oxygen and he did not survive the infection.
Myanmar’s Ministry of Health counts nearly 20,000-recorded deaths from COVID-19 up to the end of 2021 – the fourth highest mortality rate in south-east Asia. But this figure is misleading – only counting people who died in hospitals. Countless individuals, like Naung’s father-in-law, were passing away in their homes while facilities were full – we know because some of these deaths were happening in our communities and among our team’s families, and they did not make it into the official figures. The real figure we will never know, but from our experience responding to epidemics, it is undoubtedly multitudes higher.
Similarly, the military government lacked both the capacity and the trust of people to effectively scale up testing, leaving positive rates around 35-40 per cent as only those with the most serious symptoms were getting swabbed.
How did MSF respond?
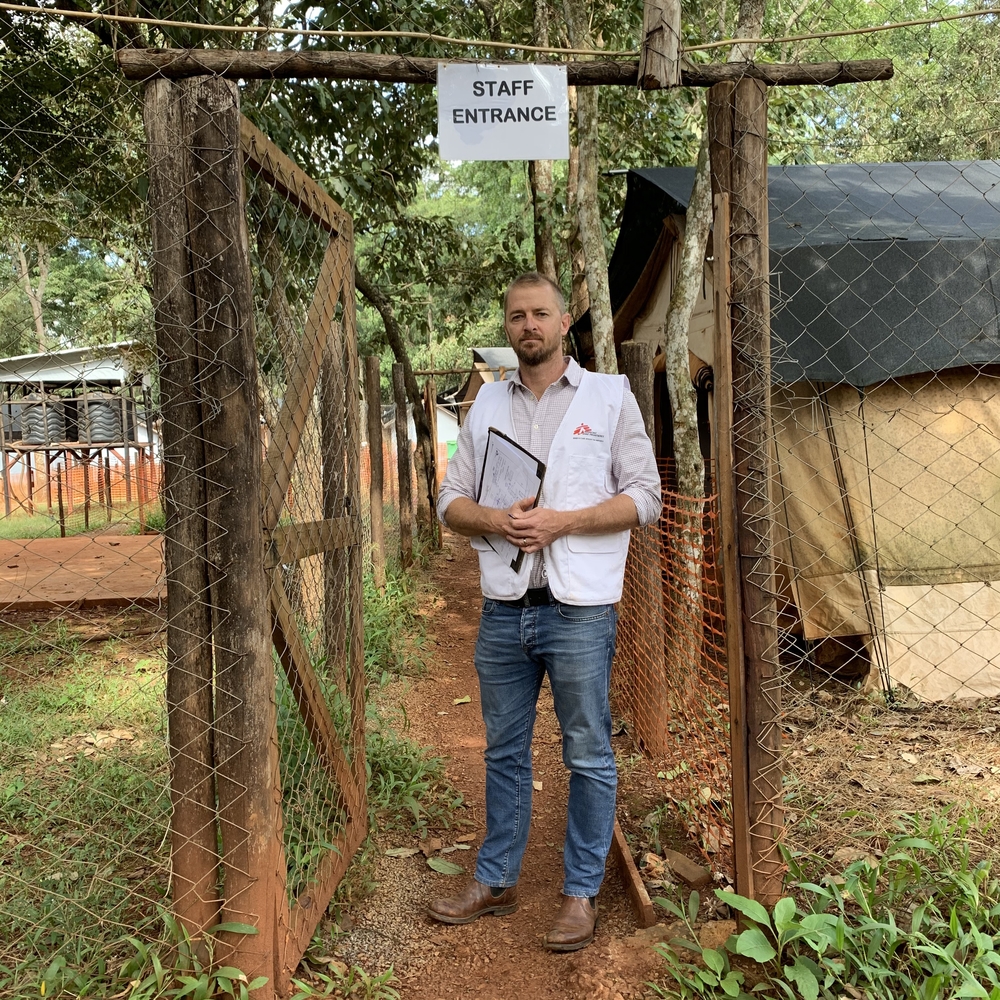
We were granted permission to open three independent COVID-19 treatment centres to receive patients with moderate to severe symptoms in Myanmar’s biggest city Yangon, and Kachin state’s Myitkyina and Hpakant townships.

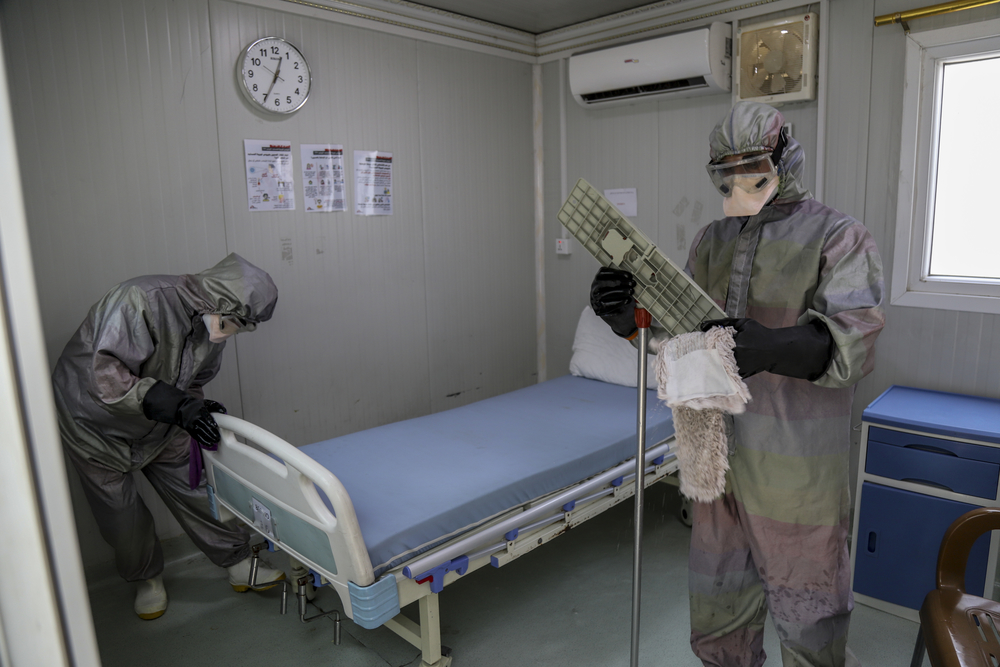
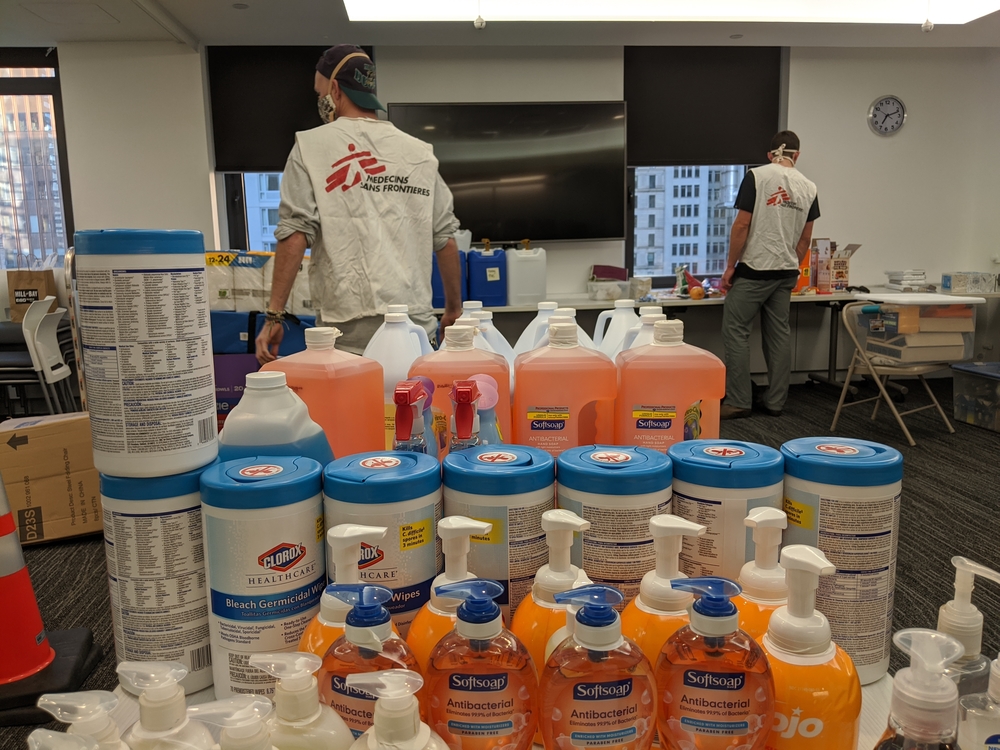
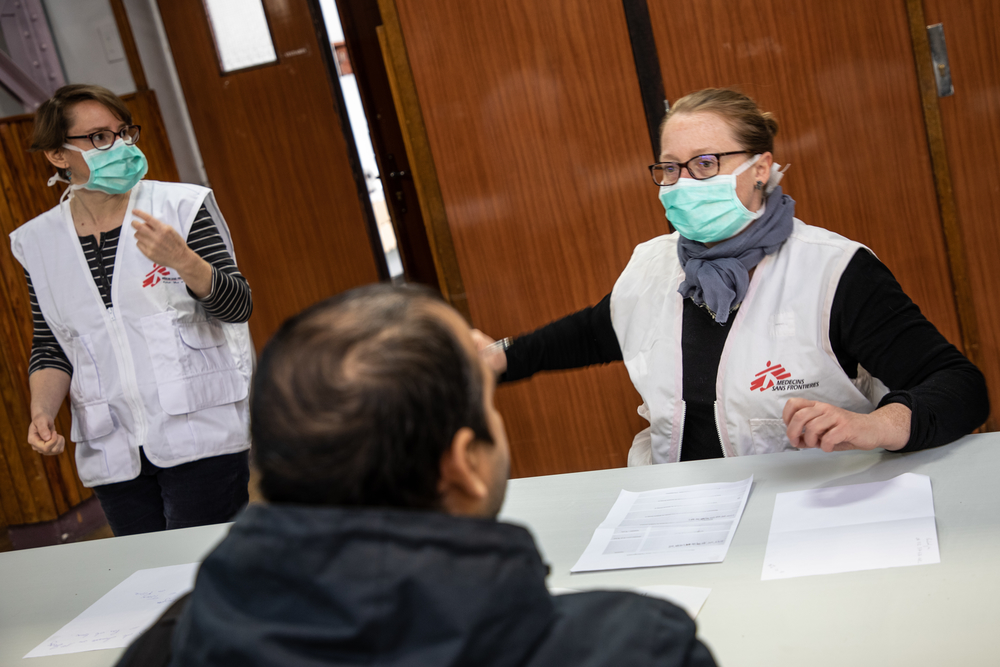
Our human resources department worked at full stretch to hire more than 150 staff in a matter of weeks. Our logistics team sourced equipment, including life-saving oxygen concentrators, and found and refurnished premises appropriate for COVID-19 patients. Our medical staff trained up teams of doctors, nurses and assistants to deliver quality care to their patients.
To do this at such a rapid pace took an incredible amount of work, particularly when COVID-19 was infecting the team and our families. Remarkably, while some of us fell seriously ill with the virus, no one on the team lost their life to COVID, but many of our family members did. Despite this, we pulled together and looked after each other, working overtime to get the centres up-and-running for people we knew were in urgent need of its services.
Although we could not save some patients admitted in very critical condition, some people made remarkable recoveries. One woman living with HIV could barely breathe when she arrived at our facility. But in five days she was off oxygen and could be discharged, making way for another patient.

For others, the progress is slow and steady. One 64-year-old woman was in our Myitkyina clinic for 46 days, slowly improving her lung capacity until her oxygen levels were good enough for her to go home.
When there are no acceptable solutions
Our response could have and should have been bigger. When cases started to appear on Myanmar’s western frontiers, MSF attempted to explore how to respond in Chin state where there was a critical lack of doctors, but authorities in the capital Naypyidaw, citing security concerns, blocked our travel plans. Transporting key medical supplies to these under-resourced areas was all we could do.
While we had permissions to run independent COVID-19 responses in three locations, not all local health authorities were on the same page.
We had begun supporting a facility in Lashio, the capital of northern Shan state, on August 11, 2021, but one person within the Lashio healthcare structure ordered us to close it down on August 15, 2021. Days after receiving our first patients, we were forced to transfer six people receiving treatment to the military government’s treatment centre despite their preference to receive care from MSF.
Did we respond in time?
By the time our first treatment centre was up-and-running in early August, COVID-19 was already devastating the country. If we were better prepared and more reactive, could we have responded sooner and saved more lives? The answer is an uncomfortable yes.

The Delta variant had overwhelmed India and Bangladesh in the months before – two countries that share a porous, 2,000 kilometre border with Myanmar. Its arrival was inevitable. We could have used that time to prepare and equip ourselves, and to have learned from the challenges MSF had faced responding in India where access to oxygen was one of the biggest issues, like it would become in Myanmar. Yet this is, of course, easy to say with hindsight.
When the third wave hit, Myanmar was six months into the military takeover. The team was already working at full stretch to maintain existing activities and fill the gaps left in the struggling public healthcare system, in particular taking on thousands of HIV patients from the state’s National AIDS Program.
We felt there was no capacity to respond to an outbreak while maintaining quality of care for patients we were already responsible for. But, as an emergency medical and humanitarian organization, this initial and well-intentioned hesitancy became an untenable position as we all watched the chaos ensue.
Yet by the time we initiated our response in the middle of July, we were already on the back foot.
We did not always get it right
There was a belief that we could simply put people on oxygen and save lives. This was not the reality of treating COVID-19 patients. Those who are hospitalized with severe symptoms often have underlying conditions, exacerbating their symptoms and complicating their treatment.

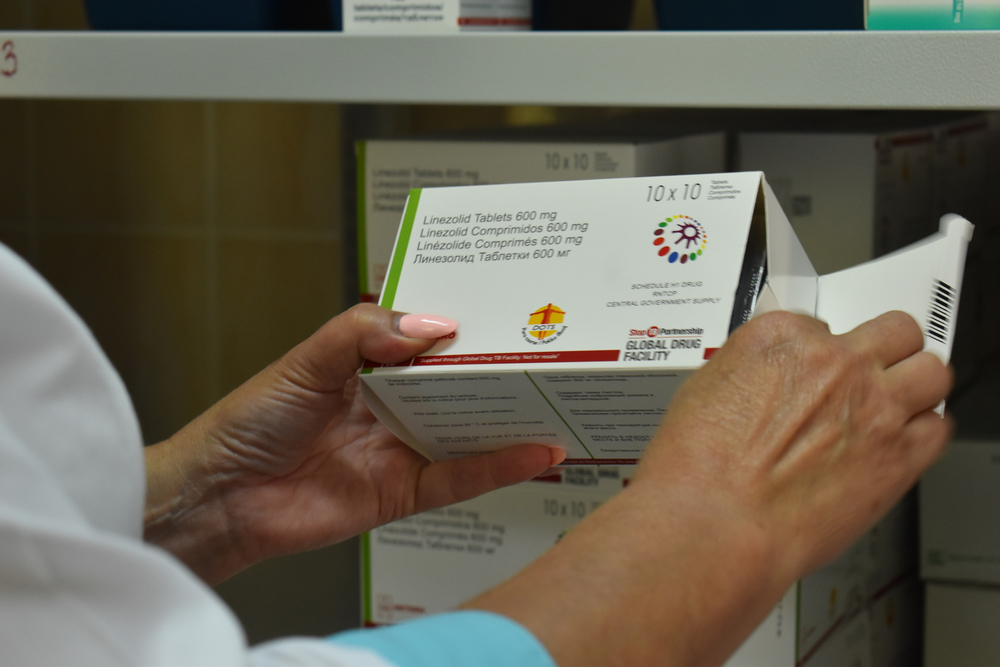
We needed essential drugs like insulin and basic cardiovascular medication, but they were not in our warehouse and we could not get them into the country due to convoluted internal processes and difficulties obtaining import permits. We had an emergency preparation kit for COVID-19, but what we had expected to be there was missing, such as medicine to treat blood clots, and the supplies that were included were quickly exhausted. When we were trying to buy them in Myanmar, the third wave had already gripped the country and these vital drugs were in high demand and short supply.
Committed and ready
Although internal and external constraints and challenges caused difficulties, our COVID-19 facilities are now much more than field clinics – they are excellent hospitals that have saved many lives and will save many more to come.
Only around 13 million people in Myanmar are fully vaccinated – around a quarter of the population. If another wave of infections spreads, the public healthcare system risks being overwhelmed once again.
With that in mind, we are maintaining our COVID-19 infrastructure and keeping medical staff on-hand should there be another outbreak.
Although our supplies of essential medicines have improved, importing them remains an issue. Permissions are currently under more scrutiny than prior to the military takeover, delaying shipments. Furthermore, internal MSF processes and policies for local or regional procurement of medicines have not adapted well to the global supply crisis and often hinder emergency purchases.
We have learned many lessons from the challenges we faced the first time round. We remain committed and ready to respond to new and unexpected challenges to come. Our commitment to the people of Myanmar is unwavering.
Sincerely,
The MSF Myanmar team