COVID-19 response in Kenya
By Lili-Marie Wangari, Emergency Preparedness Coordinator for Doctors Without Borders/Médecins Sans Frontières (MSF) in Kenya. Wangari is working on the organization’s response to the COVID-19 outbreak. This includes providing support to a health centre and to community health efforts in Kibera, one of the largest slum settlements in Africa. There are currently 320 cases in Kenya, with the majority concentrated on the capital, Nairobi. Here she explains her work to help to protect some of the most vulnerable people within the city.
When we heard about COVID-19 we reached out to the Kibera South Health Centre. It’s a facility that MSF built and managed, before handing it over in mid-2017 to the Ministry of Health to continue to run.
Kibera is a community we know well – we worked there for more than 25 years, through the HIV/AIDS crisis in the 1980’s, when we cared for people at home, campaigned for access to treatment and were the first doctors to provide antiretroviral drugs to patients in a Kenyan public health facility.
Because we know Kibera, we know how catastrophic an outbreak could be in the community.
Lack of resources make preparation difficult
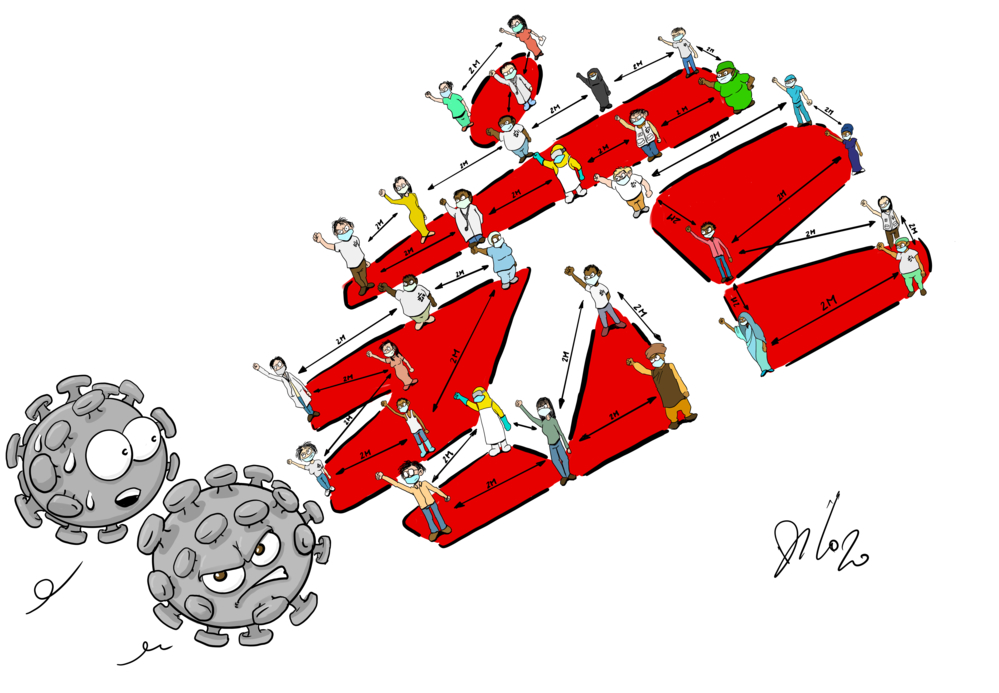
Maintaining physical distance in Kibera is almost impossible, as it is in many slum settlements around the world. People live in tiny, overcrowded homes with few windows or other ventilation. These conditions, as well as making it easy for a disease like COVID-19 to spread, make it very difficult for people to stay inside for long periods of time.
Access to water is extremely limited, with only 200 water points for the approximately 200,000 people who live in the settlement, making regular hand washing almost impossible.
In this environment, the usual health promotion messages just don’t apply.
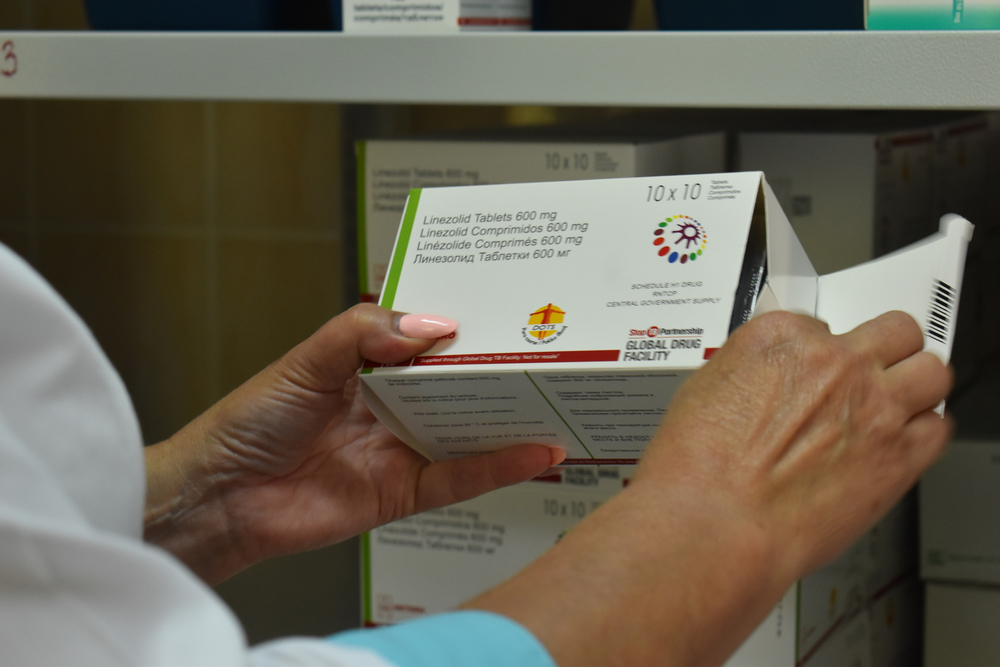
My biggest concern is that a large proportion of people have underlying health conditions such as HIV, TB and non-communicable diseases like hypertension and diabetes that could put them at an increased risk of developing severe COVID-19.
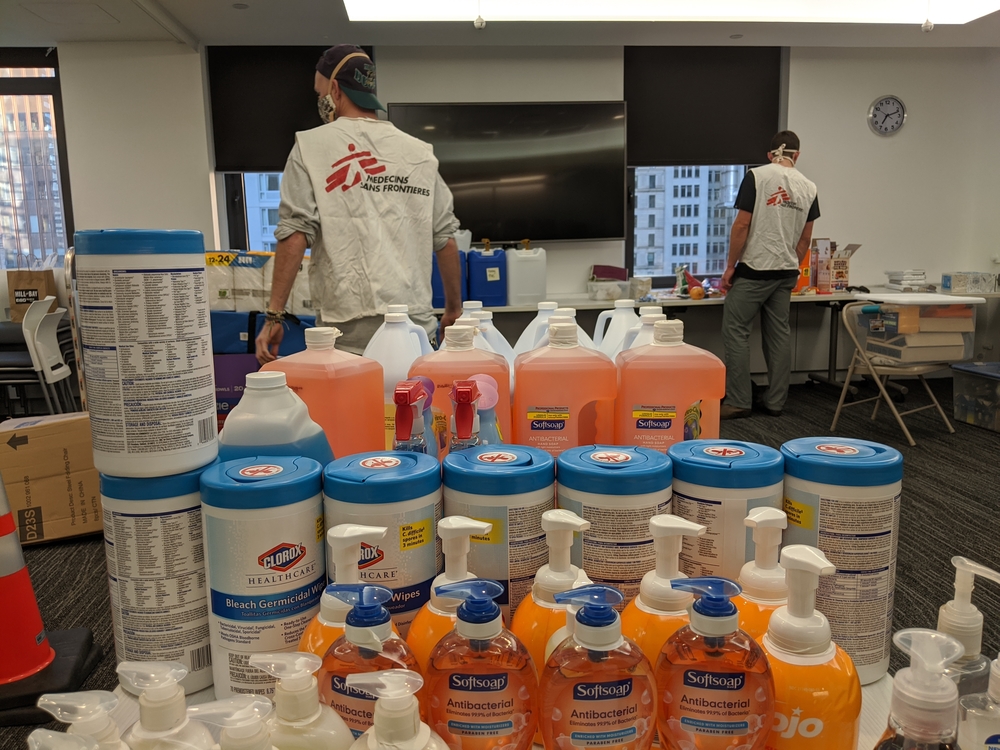
Whilst healthcare is available in Kibera, we are concerned that it might be impacted by the outbreak and reduced if health workers fall ill or supplies can’t get through. All health workers need Personal Protective Equipment (PPE) but it’s becoming expensive and is in short supply in Kenya and around the world. Even for MSF, this shortage is a huge challenge that stands in the way of us wanting to do more for the communities that we support.
There are other social or economic factors that put people at additional risk. Most live hand to mouth, day to day, so still have to try to work to have enough money to buy food. This involves travelling through the city, walking or taking public transport, including extremely overcrowded trains which cut through the slum, risking exposure to the disease.
MSF in Kibera
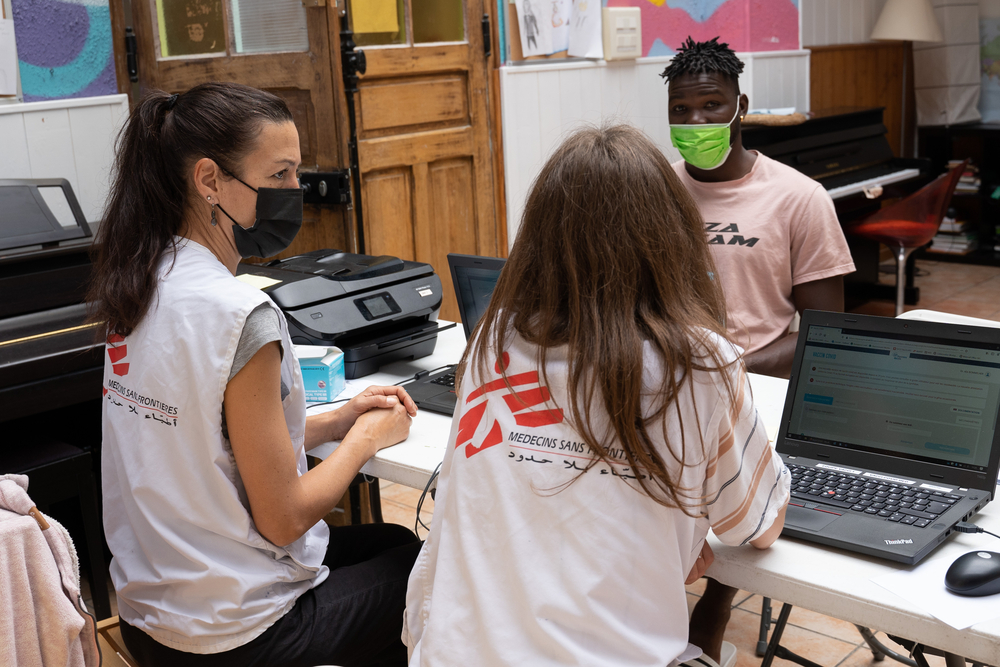
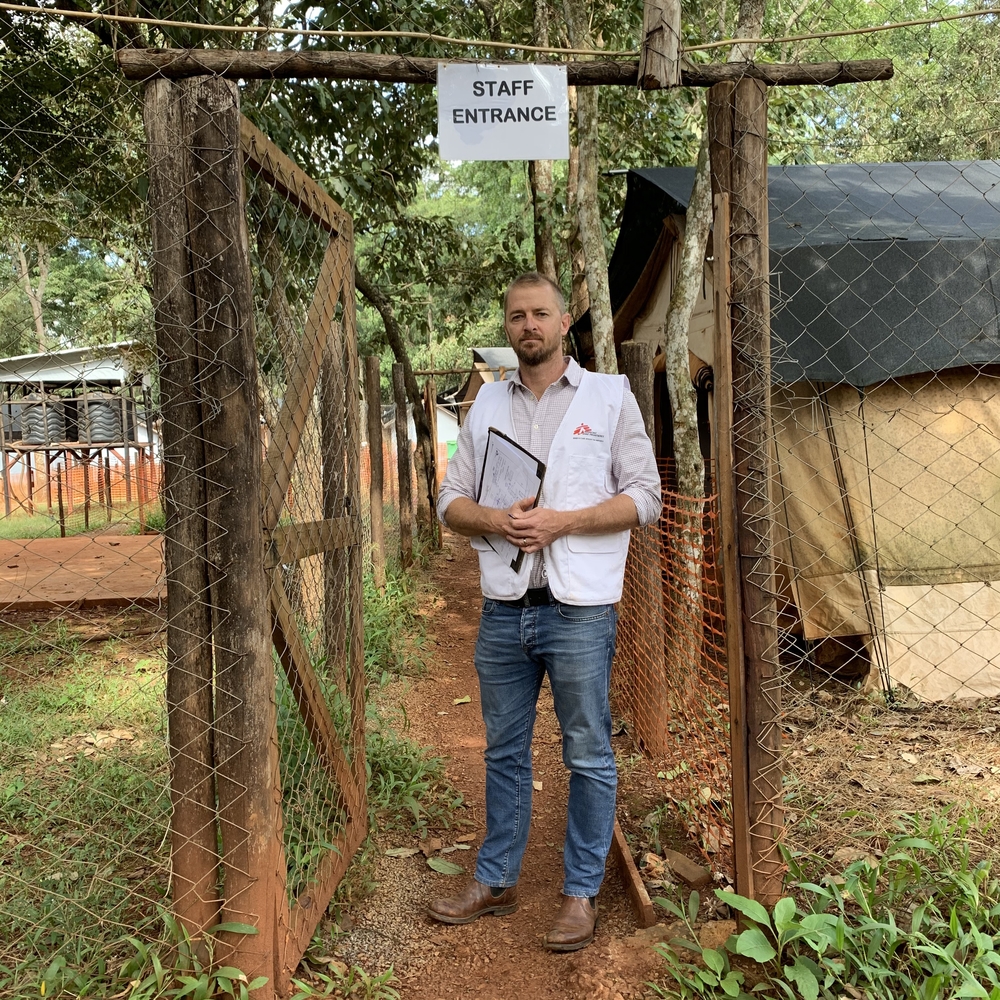
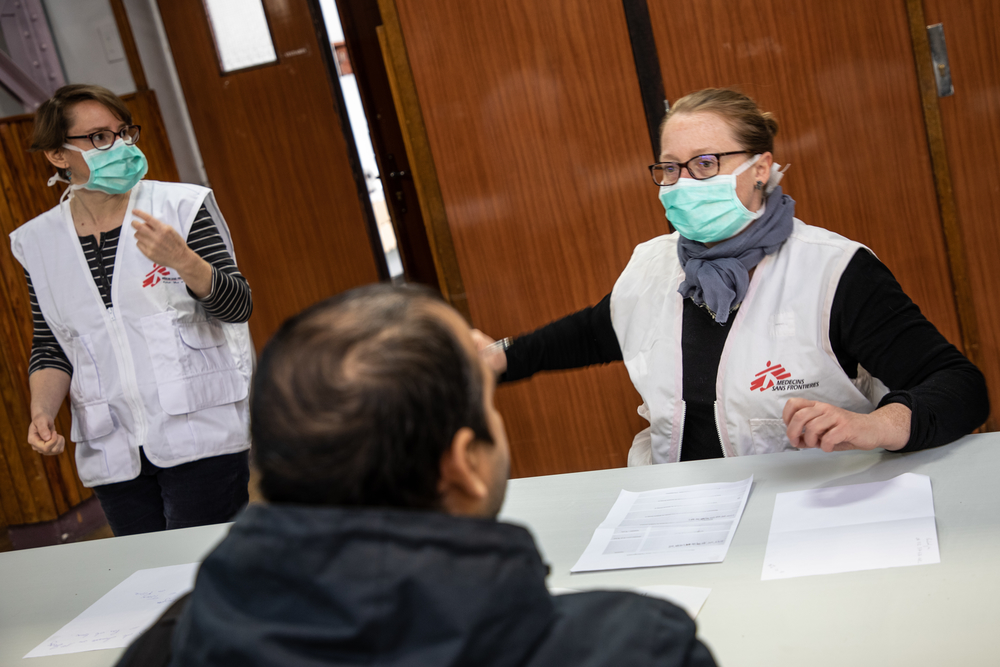
For the past two weeks, a team of seven MSF staff have been working back in our old health centre. They have set up a screening system, run by two community health workers in a tent at the clinic’s entrance, who take patients’ temperatures and control the number of people who come into the health centre at any one time.
Another community health worker and a nurse help with the screening system to make sure the flow of people is safe and that they remain a safe distance apart.
Should people have a fever, they go to see an MSF nurse for a more in depth health check.
We also have clinical officer who manages an isolation room for suspected cases which has two beds; this is where people will wait before they are referred to the government hospital for testing and treatment if necessary.
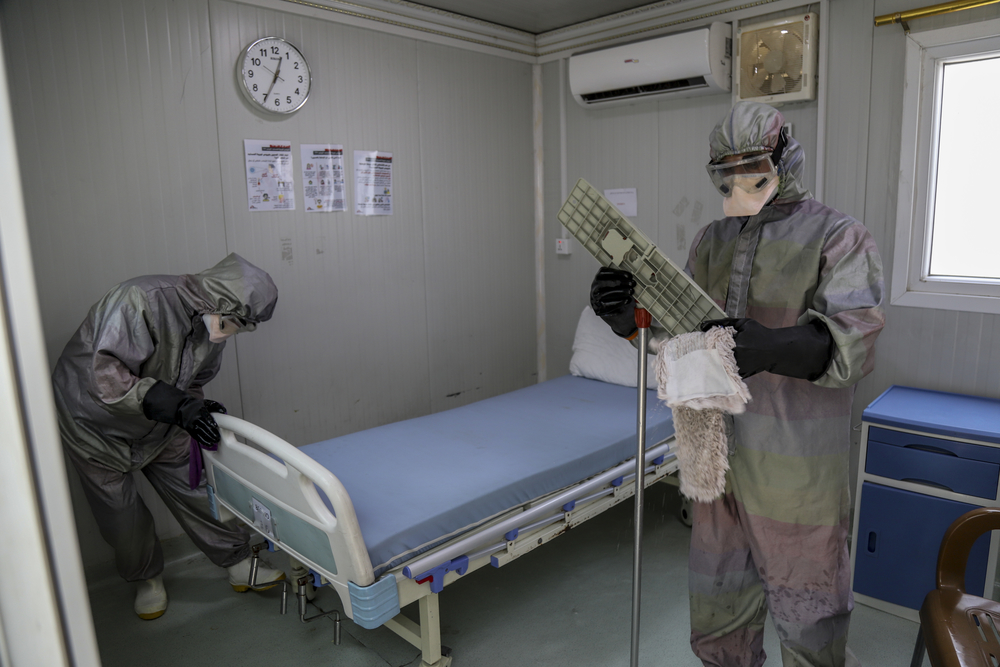
team members are also providing training and support for infection prevention and control measures. This includes making sure staff are wearing the correct Personal Protective Equipment, such as masks and gloves, and that there is a constant supply of water for hand washing.
A dedicated clinical hygiene officer is making sure high risk areas are kept clean.
As well as making sure patients are safe in the facilty, we want to protect health workers – without them, there will be no response to COVID-19 and we could see a rise in deaths from unrelated health conditions that people could not find treatment for. In our work outside of the health facility, we still have to advocate for healthcare in Kibera to continue. Diseases will not wait.
Our community health team will also be spreading health awareness messages, and are working with other groups in Kibera to install water points to improve people’s ability to wash their hands.
Moving around the community, what we hear from people is that, as well as struggling with the economic impact of the outbreak, they are scared. We already hear reports of the community rejecting people who they think might have COVID-19 and I’ve heard people shouting corona at the MSF car when I’m on the way to the clinic. There is a lot of misinformation out there that we will have to try to correct in the days to come.