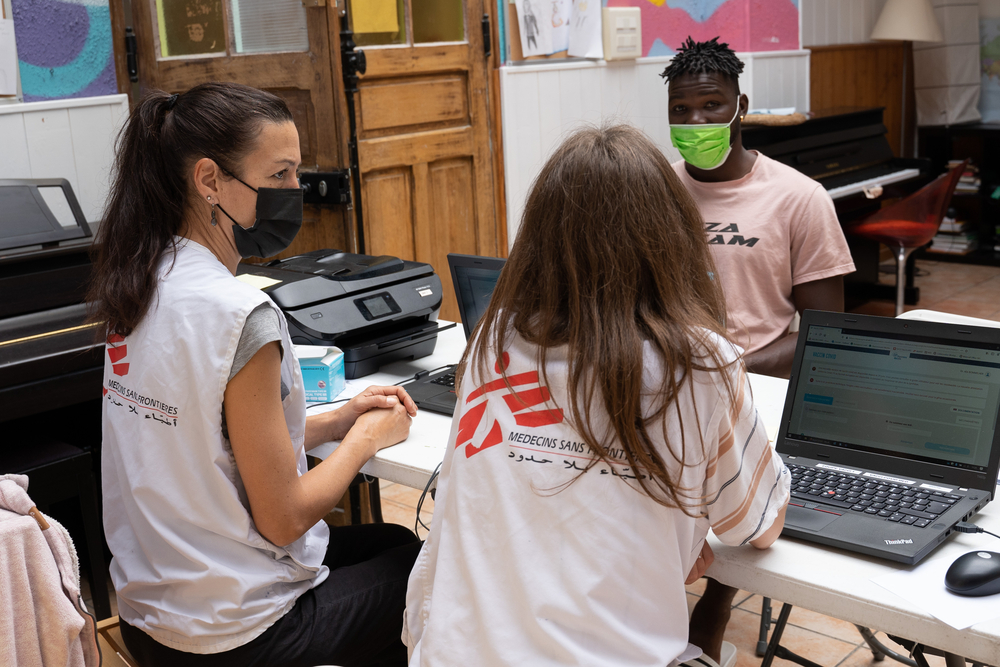
COVID-19 in El Salvador: MSF warns of increase of deaths and collapse of health system
Doctors Without Borders/Médecins Sans Frontières (MSF) has warned of an increase in people dying of COVID-19 in the metropolitan area of San Salvador, the capital of El Salvador.
“We are already at a critical stage. We are seeing an increase in the number of people dying in their homes before our ambulance services arrive. Admitting patients to hospitals has also become more difficult. Worryingly, community leaders are reporting deaths in their communities, some of them related to the suspension of primary health care,” said Luis Romero Pineda, MSF’s project coordinator in El Salvador.
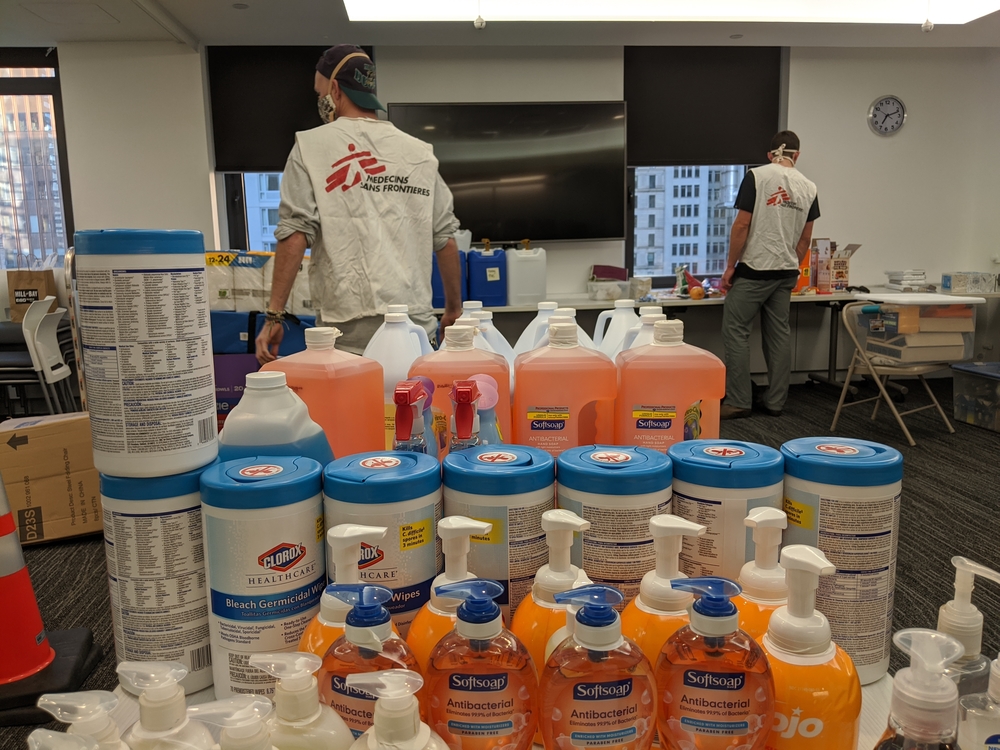
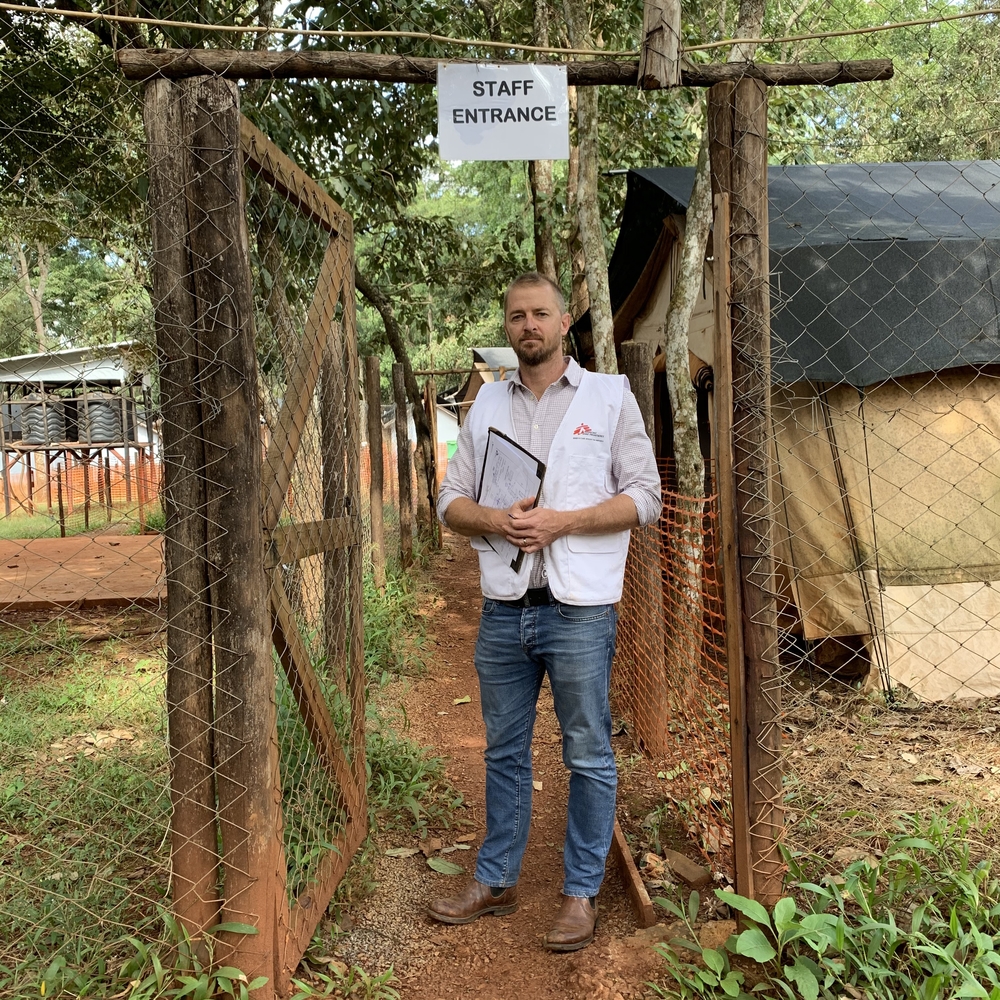
MSF has continued to run healthcare activities in Soyapango and San Salvador during the pandemic, even though the Salvadoran Health Ministry suspended most primary healthcare services in March. These cities are the most populated in the country and have become the epicentre of the pandemic. MSF has witnessed rapidly worsening conditions related to the effects of COVID-19 on people’s health and the health system is close to collapsing.
Death before hospital arrival
MSF ambulance teams in the eastern metropolitan area in San Salvador, are recording an increase in patients dying at home before the ambulance arrives. We are also receiving worrying reports about the situation in some communities in San Salvador and Soyapango.
Angel Sermeño, MSF’s medical activity manager in El Salvador, warned that “in many instances the patient had already died when we arrived at their house. In 2019, this happened to us eleven times from January to June. In the same period this year, it has happened to us 37 times, and 18 times in June alone.
According to Sermeño, “the main causes of death are related to metabolic disorders and respiratory and heart problems”, which have increased fourfold compared to the first half of last year. “In addition, there are four cases of respiratory complications that could be related to atypical pneumonias or COVID-19,” he explained.
The increase in household mortality reflects the enormous burden of COVID-19 on the health system. Based on the analysis of data from our ambulance system, there are three factors that explain the increase in mortality in recent months:
- The lack of access to primary healthcare services, which has contributed to the deterioration of the health of patients with chronic diseases.
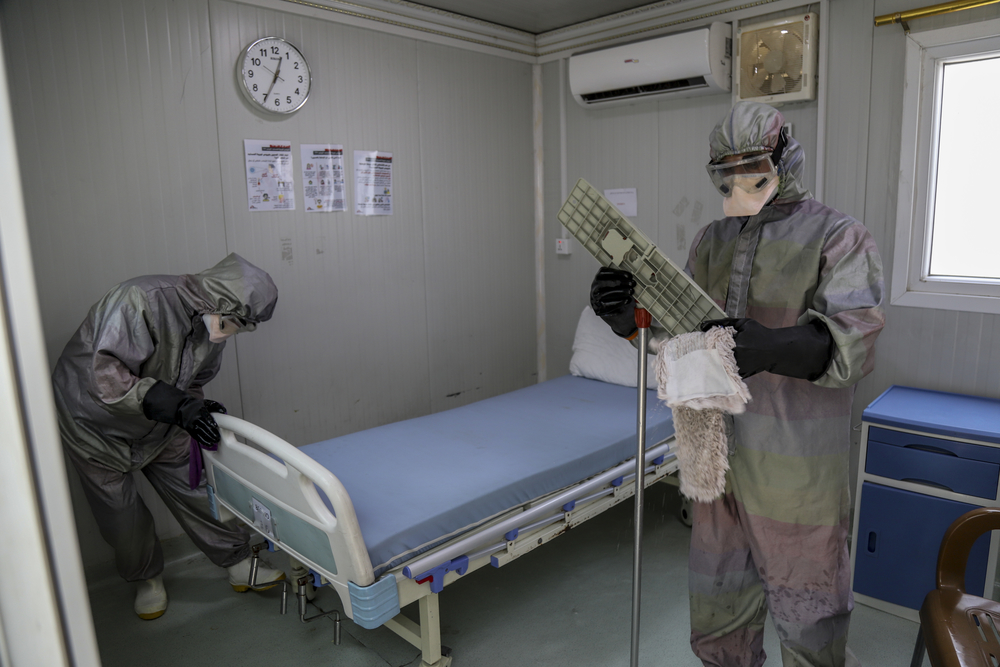
- Secondly, the ambulance system and hospitals are operating at full capacity.
- Thirdly, the mechanisms for detecting cases of COVID-19 in some communities are not systematically transferred to the national territory, which prevents the timely detection and hospitalization of people with complications.
Community leaders in the five communities where MSF provides primary healthcare in Soyapango and San Salvador, report that since the emergency was declared, more than 50 people have died after showing symptoms compatible with COVID-19 or from a lack of treatment for chronic diseases.
Many of MSF’s ambulance callouts in recent months have been related to respiratory diseases. In several cases, the ambulance was called when patients were already in a particularly serious condition.
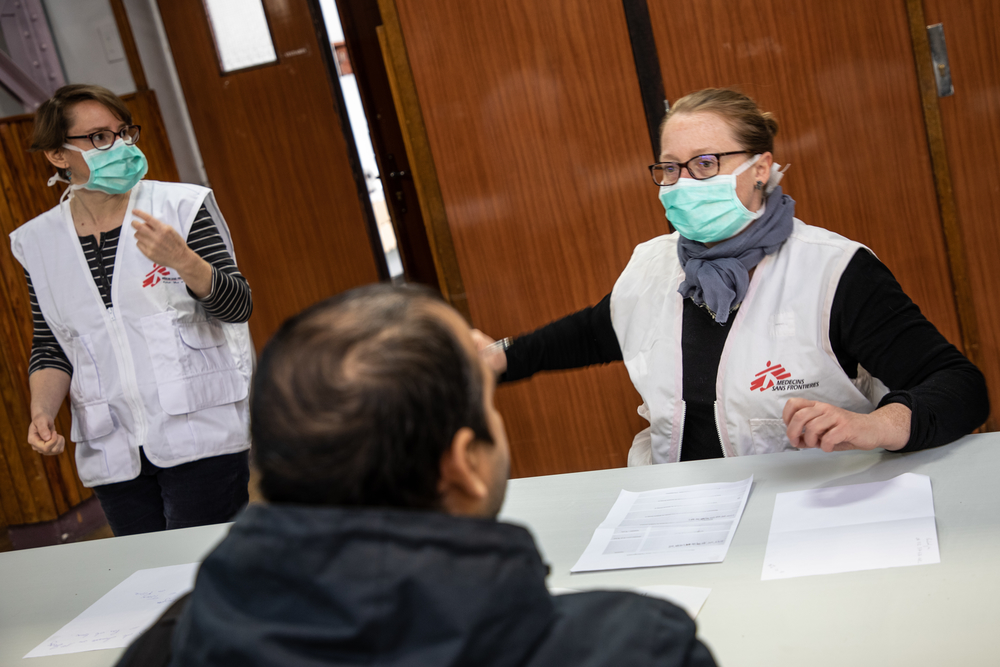
Stigma and fear of contagion are delaying people from seeking medical assistance, sometimes with fatal consequences. Many people are afraid to leave their homes for fear of being judged for carrying the disease or being taken away from family members if they are hospitalized.
Some people cannot even afford a mask, and others seek help but are not attended to due to the suspension of consultations and infection controls in hospitals and health units. Victor, a patient from Soyapango, told MSF how his grandfather has chronic health problems and has to change his catheter every few months, “We took him to a hospital in San Salvador where he was asked to go to one in Soyapango, and from there, to another. They have already told him that it is better not to go to get the catheter, that it is better not to go out, that there is no equipment to treat to him“.
Wendy, a doctor working in MSF’s ambulance service, explained how some patients die while waiting to go to hospital because, “we have to wait for authorization from the public health system to be able to move patients to a care centre, since we cannot transfer the patient from his or her home without prior coordination and authorization from the public health system.”
“It is vital to improve coordination, increase the number of available beds and ensure protective measures in hospitals to guarantee the safety of staff and patients, as well as increase the response capacity of the emergency transfer services in critical cases,”, says Romero Pineda. “It is also essential to guarantee access to primary health care and improve case detection and follow-up to prevent cases from becoming serious, whether they are COVID-19 or not”.