MSF: Immediate equitable access to COVID-19 vaccines is critical for Southern Africa and the world to prevent more suffering and death
Urgent action is required of leaders of wealthy nations, pharmaceutical corporations and COVAX before it is too late.
As COVID-19 continues to sweep across Southern and Sub-Saharan Africa, aggravated by a highly infectious variant of the virus in strained, fragile healthcare systems, equitable access and distribution of vaccines is more critical now than ever.
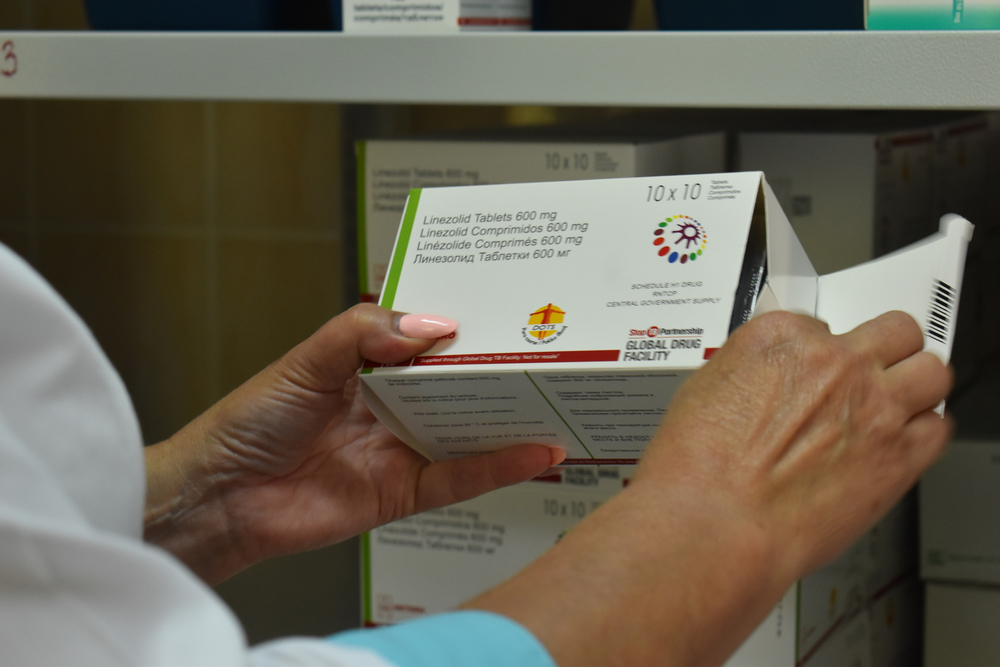
With the latest initial data indicating that some COVID-19 vaccines may be less effective than others against the 501Y.V2 variant first discovered in South Africa, Doctors Without Borders/Médecins Sans Frontières (MSF) is calling on wealthy states and pharmaceutical corporations for solutions that will urgently ensure that all countries can access effective vaccines quickly and affordably – before it is too late.
“The emergence of new COVID-19 variants should be a major consideration in determining the allocation of vaccines to countries around the world. We have already seen South Africa forced to halt and adapt its planned vaccine rollout of one particular vaccine due to findings indicating decreased efficacy against the dominant 501Y.V2 variant,” says Dr Tom Ellman, Director of MSF’s Southern Africa Medical Unit.
“Truly equitable vaccine allocation and distribution should mean that countries are able to acquire not just any vaccines but the right vaccines – adapted to the presence of new variants and to contextual factors- at the right time and at the right price. Unless the leaders of wealthy states and pharmaceutical corporations support this, and quickly, we risk generating new pandemics of vaccine-resistant COVID-19. Travel bans will not stop this but equity and solidarity might,” continues Ellman.
After a scramble last week, South Africa acquired a different trial vaccine to ensure its most-at-risk frontline healthcare workers get protection in a limited rollout as part of an implementation study, starting this week. However, it is clear that accessing vaccines for low- and middle-income countries will remain a serious problem unless systemic issues linked to protectionist agreements between wealthy nations and pharma corporations are dealt with. South Africa is now offering to share its initial unused vaccine consignment with the African Union for use in appropriate countries where the 501Y.V2 variant is not predominant.
To date, more than 174 million people globally have been vaccinated, and almost none of these have been in Africa. Moreover, many developed countries have ordered two to three times as many vaccines as are actually required by their populations, and some are even set to receive vaccines from COVAX, which many developing countries exclusively rely on for vaccine access. Aggravating the situation, these same countries that have already vaccinated many of their healthcare workers have for months blocked efforts led by South Africa and India to waive intellectual property protections on COVID-19 medical products, including vaccines, at the World Trade Organization (WTO). This move could enable low- and middle-income countries to produce or access these products more affordably through technology transfers, increased local manufacturing and price competition in the medium term.
“What we are witnessing right now is an unacceptable failure of humanity and the global response. We denounce countries that hoard vaccines and who have started to immunise low-risk groups since it comes at the expense of developing countries who haven’t even started vaccinating frontline healthcare workers in health facilities already stretched to the breaking point,” says Claire Waterhouse, MSF’s Regional Advocacy Coordinator.
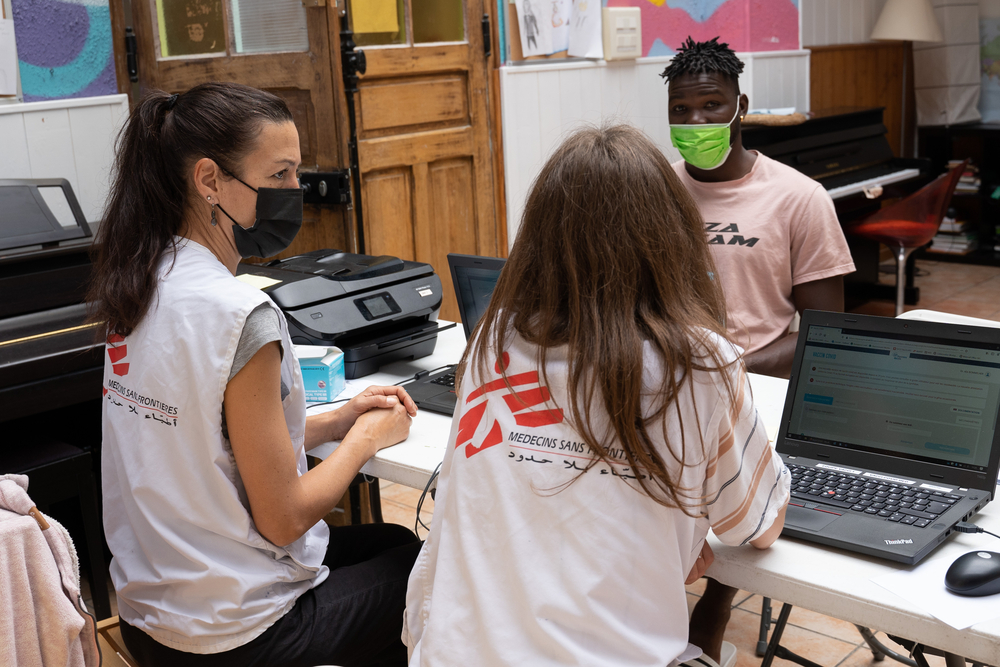
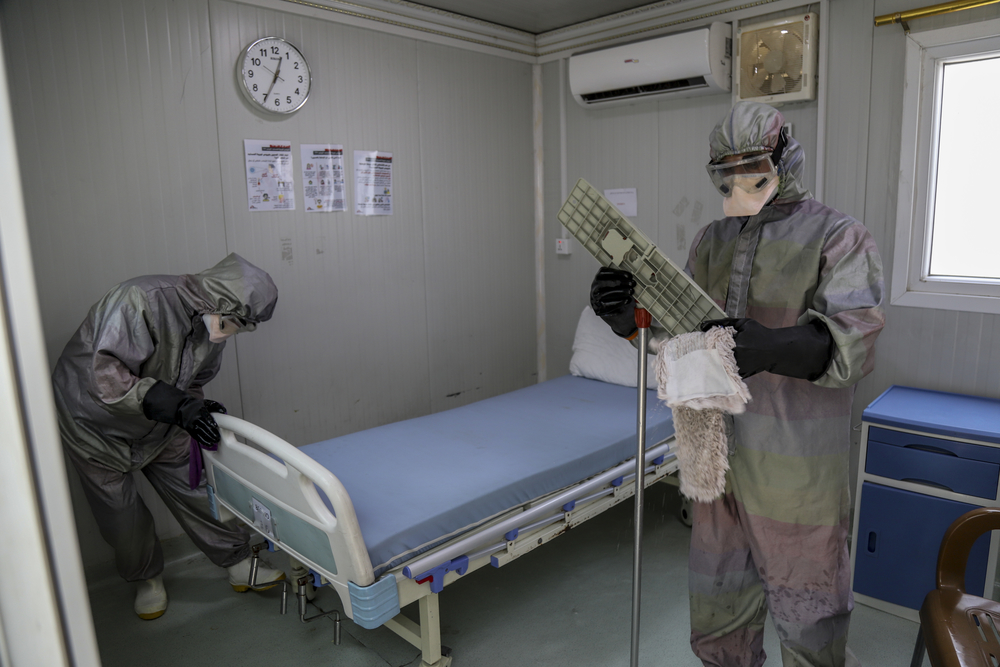
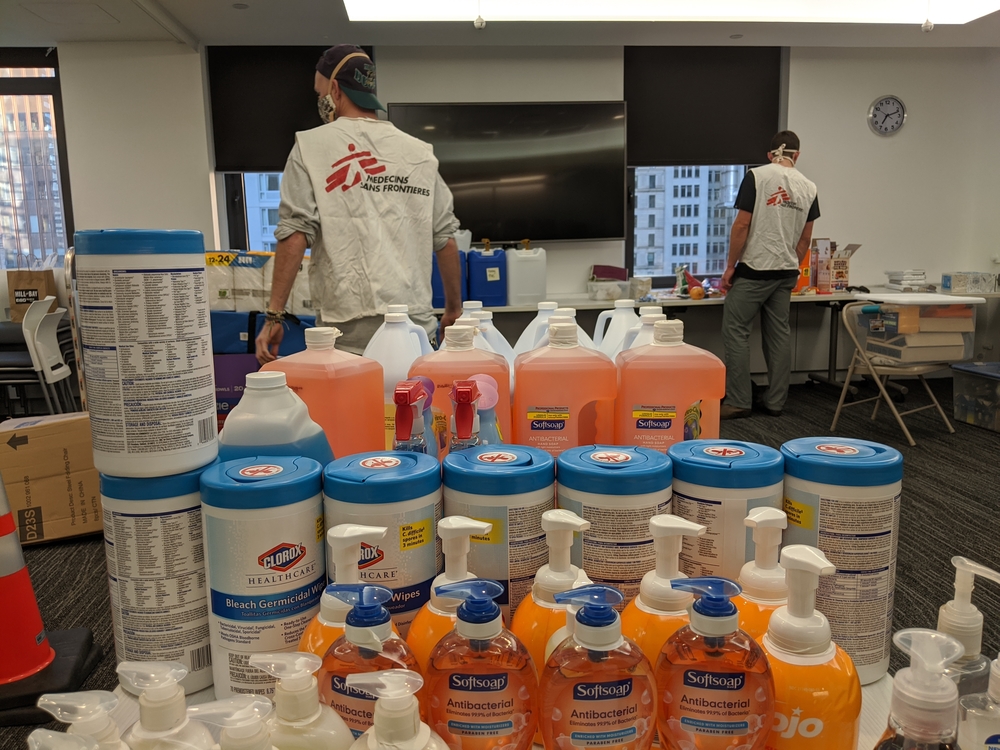
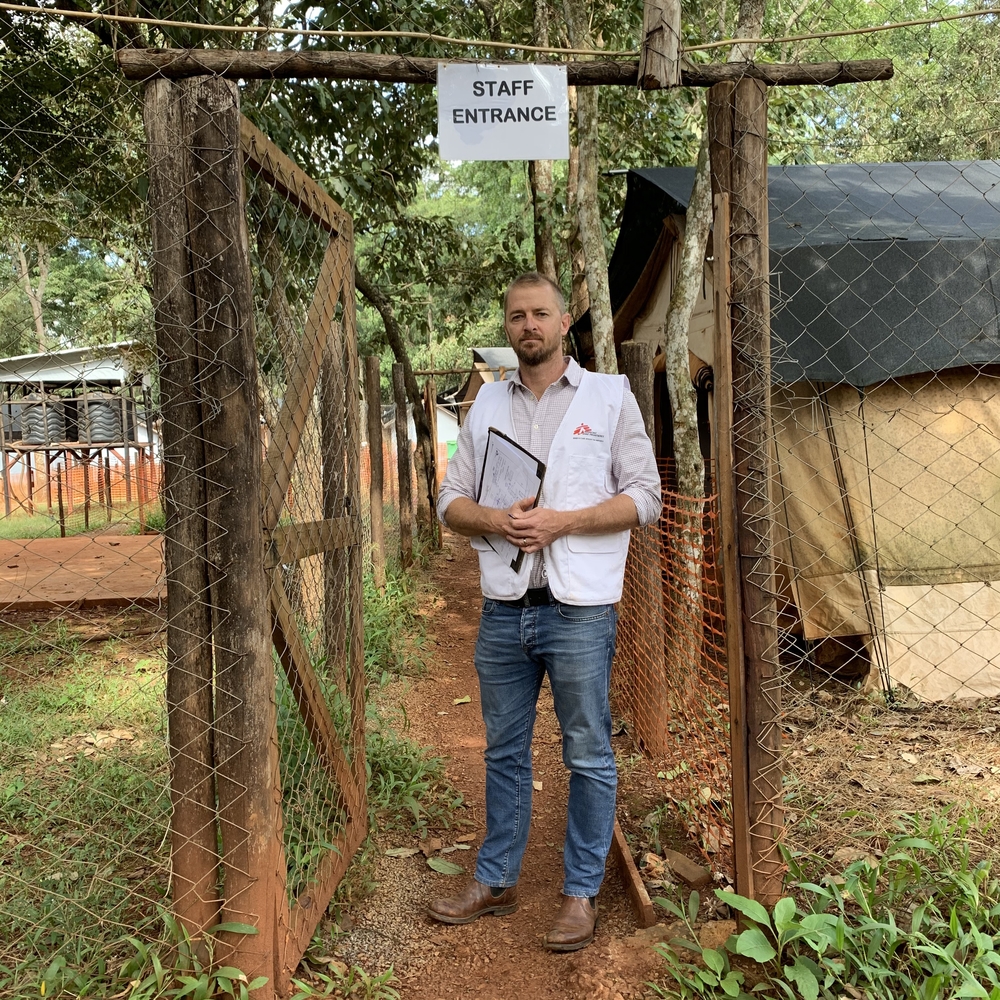
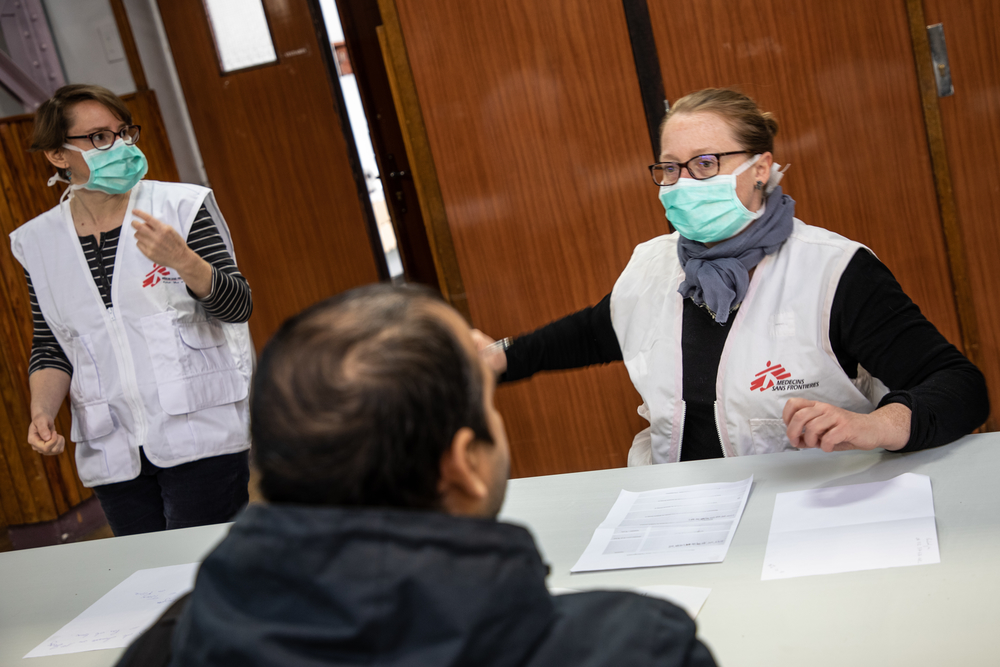
MSF teams have been providing COVID-19 treatment and prevention in different communities throughout Southern Africa – in Eswatini, Malawi, Mozambique, South Africa, and Zimbabwe – since the beginning of the pandemic. Following the festive holiday season, the region was shaken by a sudden ‘second wave’ of COVID-19 infections. Several Southern African countries recorded more new COVID-19 cases in the month of January 2021 than in all of 2020.
“MSF staff have witnessed the severe impact of the ‘second wave’ on this region, its people and its health systems, which struggled to cope with the sudden onslaught of patients. In South Africa, there weren’t enough healthcare workers in many of the hotspots and hospitals struggled to meet the demands for care,” explains Philip Aruna, MSF’s Regional Operations Manager in Southern Africa.
“While the wave of new infections is starting to slow in some of these countries, we are now preparing for the possibility of future surges of COVID-19 infections as the virus continues to adapt and spread. A quick rollout of the most-effective-in-context vaccines would have a significant impact on reducing future infections and deaths among healthcare workers and most at-risk-groups. However, most countries in Southern Africa, and indeed the developing world, have yet to receive the quantities of vaccines they need,” Aruna concludes.
The system of access to medicines and vaccines needs to change at all levels. The solution to get ahead of the global danger of COVID-19 is for the leaders of states and pharmaceutical corporations to act urgently on the fact that until everyone has access to the right vaccines for their reality, all countries will pay the price.
- MSF urges governments of wealthy nations that have immunised their frontline healthcare workers and high- risk groups to now help low- and middle-income countries by sharing their supplies with COVAX.
- Additionally, MSF urges pharmaceutical corporation leaders to pause or stop bilateral agreements that would over-supply wealthy nations hoarding vaccines in order to prioritise the supply of vaccines to the COVAX facility or bilateral deals for countries yet to vaccinate their healthcare workers and high-risk groups.
- MSF calls on COVAX leaders, GAVI – the Vaccine Alliance, the Coalition for Epidemic Preparedness Innovations, the World Health Organization and donor states, to take immediate steps for speedy transparency on COVAX supply schedules, so that low- and middle-income countries know price, quantities and delivery date of vaccines they will receive.
“While the COVAX mechanism is designed specifically for equitable distribution and vaccine development, it has yet to deliver a single vaccine to a country. COVAX lacks crucial transparency toward participating countries. It is clear that the global vaccine access system is inherently flawed, and we urge GAVI and donors to COVAX to acknowledge this and take steps to address this,” says Waterhouse.
“They must act now! Every day COVID-19 vaccines are delayed is another day that healthcare workers in southern Africa and developing countries remain at great risk while they continue to care for the sick.”